#9: Itching
Age, G/P, relationship status, occupation: 49 year old, G3P3 (Cesareans), married, administrative assistant at a large university
Menstrual status: s/p hysterectomy at age 33
Contraceptive method: N/A
Sexuality status: Male partner. Sexual intercourse comfortable and enjoyable.
Chief complaint: Years of vulvar itching.
Symptoms (HPI: history of present illness): The itching began shortly after her hysterectomy, which was done for fibroids when she was 33 years old. (She had a bilateral oophorectomy ten years later for ovarian cysts). She often felt rawness, which was aggravated by urination. She was treated for Candida and atrophy without success. Symptoms worsened after a trip to India years ago, with treatment for severe diarrhea with antibiotics. Back in the USA, she was treated for yeast and then had a vulvar biopsy five years ago showing dermatitis. Clobetasol irritated her. Vagisil and Gynelotrimin brought slight temporary relief.
Lifestyle issues: uses only pure and natural products, although she does use Vagisil
History and review of systems:
- Vulvovaginal history: yeast infections?
- GYN history: TAH for fibroids, age 33, BSO age 43 for ovarian cysts; no abnormal Pap smears.
- Past and current medical conditions: bone spur, obesity, mitral valve insufficiency, cardiac arrhythmia, osteoporosis, osteoarthritis, plantar faciitis, chondromalacia, chronic anxiety, eczema.
- Past surgical history: tonsillectomy, three cesarean sections, tubal ligation, appendectomy, hysterectomy, bilateral salpingo-oophorectomy.
- Associated review of systems:
- Urinary: pain with urination, frequency, nocturia
- Gastrointestinal: negative
- Musculoskeletal: arthritis in knees
- Dermatological: itchy patches over elbows and flanks
- Other review of systems: environmental allergies
Medications:
- Glucosamine
Allergies:
- Cyproheptadine
- Ampicillin
- Erythromycin
- Cephalosporins
KEY POINTS FROM THE HISTORY:
- This is chronic itching in an atopic individual.
- Biopsy did not clearly direct care and clobetasol brought no relief.
Non-genital exam:
BMI: 32.5 kg/(m^2); vital signs within normal range.
GENERAL: obese female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Dry, with excoriations under the breasts. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Very itchy on thighs. Skin dry, but otherwise normal in appearance.
Genital exam with symptom mapping:
Exam: well tolerated.
Groin: itchy. Skin appears normal in texture and integrity.
Mons pubis: normal, non-tender. Itchy.
Labia majora: hypertrophied and severely lichenified with patches of excoriation from scratching. Itchy.
Perineum: normal skin color and texture and normal anatomy.
Anus: normal skin color and texture and normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: slightly flattened bilaterally, normal skin color and texture
Prepuce: normal and mobile.
Clitoris: visible.
Interlabial folds: normal skin color and texture and normal anatomy
Vestibule: non-tender to q-tip test, normal skin color and texture
Urethral meatus: normal size, normal location, no masses.
Vagina: mildly atrophic, non-tender; Discharge: scant.
Pelvic Floor: no hypertonicity
Cervix: absent
Uterus: absent
Adnexa: absent
Rectal: not indicated.

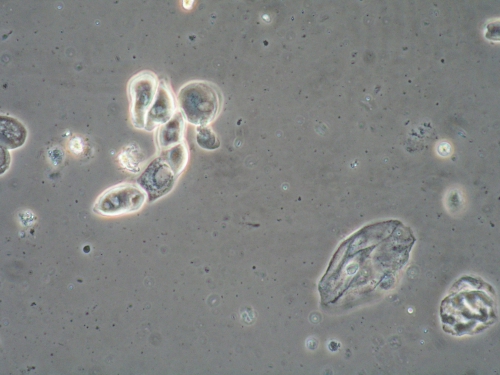
Microscopy:
Vaginal pH: 5.0
Wet prep: normal epithelial cells, 30% parabasal cells, one WBC per epithelial cell, no clue cells, no trichomonas, few lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM THE EXAM:
- The lichenification and excoriations pointed to the diagnosis.
- The biopsy result of “dermatitis” supported the diagnosis, in a way, since dermatitis, eczema, and lichen simplex chronicus look very similar histologically.
PRELIMINARY DIAGNOSIS:
- Lichen simplex chronicus
- Vaginal atrophy, mild to moderate, not causing pain with intercourse
Plan:
Testing sent or ordered: Yeast culture sent. Results: negative
Education: General vulvar care, handouts on lichen simplex chronicus and on steroid use in vulvar care. Emphasis was on need to stop scratching to make symptoms go away.
Restore epithelial barrier: soak and seal with Vaseline morning and night for seven days.
Treatment: clobetasol 0.05% ointment applied in a thin film twice daily for 14 days, then once daily for 14 days, then twice a week. Atarax (hydroxyzine)10 mg orally at bedtime for sleep. Fluconazole 150 mg orally weekly to prevent Candida albicans.
Return visit findings:
Eight weeks later:
Initially her symptoms came into control, but they returned when she stopped the therapy. A bad flare occurred after antibiotics were taken for dentistry. She resumed clobetasol, but was itching all over her body. Culture was positive for Candida albicans. She developed a rash from fluconazole. Gynelotrimin was of no help. Lidocaine burned. She could not sleep with doxepin or Benadryl. She was diagnosed with neuropathic itching and started on gabapentin. This sedated her.
Sixteen weeks later:
She was evaluated by Dr Lynette Margesson, vulvar dermatologist, who diagnosed lichen simplex chronicus with chronic contact dermatitis, secondary infection, background of atopy, and vulvodynia. She was treated with an injection of triamcinolone (Kenalog) 80 mg IM, soak and seal with Vaseline, a tapering course of clobetasol and topical nystatin, a course of oral clindamycin twice a day for one week, hydroxyzine 10 mg orally at bedtime, and gabapentin. Her symptoms improved, then returned when she stopped therapy. She resumed treatment and again came into control.
Years later:
She continued to wax and wane over the next several years, and eventually developed steroid atrophy from abuse of clobetasol on the abdomen. She was again given systemic triamcinolone IM and referred for North American Series patch testing. This revealed reaction to a number of products:
paraphenylenediamine 3+
methylmethacrylate 2+
disperse orange dye 3+
disperse blue dye 1+
ethyl acrylate 1+
Carba mix 1+
ammonium persulfate 1+
She was given very long, detailed lists of substances to avoid, plus several pages of products that would be safe for her. When she reviewed this, she realized that she would flare whenever she took Motrin, as it was orange; she also flared after Indian sweets, many of which are orange based and she stopped turmeric also.
Her itching is now largely controlled but flares when she comes in contact with her known allergens, especially orange dye.
TEACHING POINTS:
- Patch testing with the North American Series identified a number of products to avoid. This greatly enhanced her ability to heal.
- Centrally acting Gabapentin was also important in helping her to improve. We generally start this medication at 100 mg orally daily, increasing by 100 mg every five days up to a maximum of 1,000 mg (ten capsules) if tolerated well, stopping at the level at which they become comfortable. We allow patients to increase up to 3,600 mg, usually in two split doses during the day. If the medication helps to reduce neuropathic pain or itching, we have them stay on the medication for a few months, before trying to reduce it slowly, the same way they increased it.