#12: Itching and pain
Age, G/P, relationship status, occupation: 43 year old, G0, single woman, living with her male partner for two years. She works as a supervisor for a health care company.
Menstrual status: regular periods
Contraceptive method: none; wants to become pregnant
Sexuality status: male partner, sexually active, intermittently uncomfortable with intercourse.
Chief complaint: vulvar itching and pain
Symptoms (HPI: history of present illness): The patient reports that about eight years ago, she had a series of yeast infections that she attempted to treat with over the counter yeast creams, etc, without success. Her symptoms were itching, burning, and discharge. She then started to get a series of UTIs and was given antibiotics that made her more susceptible to yeast. She eventually went to a holistic doctor in California, where she was living, who diagnosed her with vulvodynia and had her make a number of lifestyle changes, improve her diet, and get acupuncture treatments. (She did a cleansing diet where she gradually eliminated sugar and wheat and milk products out of her diet, only adding them back after she felt better for a while. This diet helped her, she believes, to eventually be symptom-free for about a year and a half, during which time, she also was having pain-free sex.) At that point, she started to move back to the East Coast, which involved driving across the country on her own. During the drive, her symptoms flared again with severe itching, burning, and pain. She has learned that if she takes Amitriptyline in small amounts, it helps with the pain, so, if she flares badly, she takes 5 mg of Amitriptyline nightly for a week, then she takes 10 mg for a week, then she takes 15 mg for a week, etc, up to a max of 25 mg per day. She says, “When I get a bad flare up, I have no visual signs but my vagina feels like it is burning or swollen and it is painful, even when it doesn’t show anything.” She complains of chronic vulvovaginal dryness, both on a daily basis and with attempts at intercourse. Sex is no longer pleasurable for her. She has no libido and she just worries about whether or not she will have pain and how much and how she will get through it, etc. If they do have sex, she can not have it again within the next 48 hrs. She has been with her partner for two years. She loves him very much and she feels sad that this has happened in their relationship. To make things worse, they would like to have a baby. She has not used contraception for two years and has not conceived. Periods are regular and monthly. She wants to prioritize trying to get pregnant, but is also worried about her future if she ends up with a chronic, debilitating vulvovaginal condition. Another occasional feature of her symptoms is sudden, brief, shooting pain in the vagina via the labia minora. She also has occasional discomfort in the LLQ of the abdomen.
She has been followed by ultrasound for a probable small right ovarian endometrioma; at the time of her last ultrasound in June, there was also a question of uterine adenomyosis. The patient does have a history of endometriosis.
Lifestyle issues: Lever 2000, Always brand pads and liners, frequent wet wipes; she does not wear daily panty liners.
History and review of systems:
- Vulvovaginal history: yeast and bacterial vaginosis. No history of genital injury, trauma, sexual abuse or assault.
- GYN history: History of abnormal Paps; colposcopy done: benign, Paps normal since then; history of endometriosis
- Past and current medical conditions: hypothyroidism, endometriosis,
- Past surgical history: excision of benign breast lump, meniscus repair
- Review of associated systems:
- Urinary: negative
- GI: hemorrhoids, constipation, rectal bleeding
- Musculoskeletal: negative
- Dermatological: negative
- Mental health: concern about vulvovaginal condition
- Review of other systems: as above
- Social history: Non-smoker, occasional alcohol; no recreational drugs; exercises at the gym and walks to work
Medications:
- Levothyroxine 125 mcg orally daily
- Anusol 25 mg rectal suppositories prn for hemorrhoids
Allergies:
- Penicillins
- Sulfa
KEY POINTS FROM HISTORY:
- The recurrent nature of her symptoms brings the possibility of herpes simplex to mind.
- Her mounting discomfort with intercourse and her coinciding loss of libido point to possible pelvic floor dysfunction (hypertonicity) related to fear of pain.
Non-genital exam:
BMI: 26.59; Vital signs within normal range.
GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Mons pubis: normal, non-tender; anterior commissure: normal skin color and texture and normal anatomy; The patient points to this area as being where she feels a lot of itching at times (anterior commissure).
Groin: normal skin color and texture
Labia majora: normal skin color and texture.
Perineum: normal skin color and texture and normal anatomy.
Anus: normal skin color and texture and normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: normal architecture bilaterally, normal skin color and texture
Prepuce: normal and mobile.
Clitoris: visible.
Interlabial folds: normal skin color and texture and normal anatomy; the patient points to this area, bilaterally, as being where she often feels dryness and pain.
Vestibule: non-tender to q-tip test, normal skin color and texture;
Urinary meatus: normal.
Vagina: well estrogenized, not inflamed and non-tender; Discharge: normal and white.
Pelvic Floor: there is no hypertonicity. The pt tolerates two fingers for the bimanual exam well and does not mind deep palpation of the pelvic floor posteriorly. However, she may still be having some situational hypertonicity related to intercourse.
Cervix: no lesions, no cervical motion tenderness.
Uterus: midline, mobile, smooth, non-tender, not enlarged and anteverted.
Adnexa: not enlarged, no masses felt, non-tender.
Rectal: not indicated.

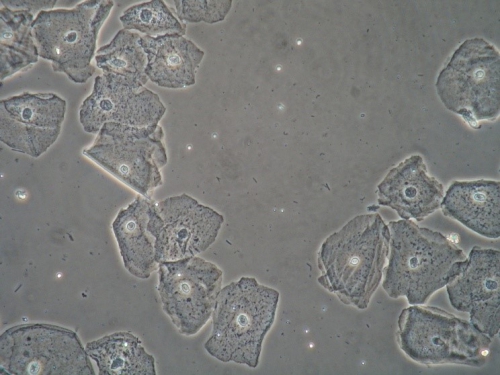
Microscopy:
Vaginal pH: 4.0
Wet prep: normal; one WBC per epithelial cell, no clue cells, no parabasal cells, no pathogens, normal lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM EXAM:
- Given the completely normal exam, including normal pH and wet prep and absence of pain with symptom-mapping, current yeast infection, BV, vulvodynia, and dermatosis are ruled out.
PRELIMINARY DIAGNOSIS:
- Possible recurrent genital herpes simplex
- Probable pelvic floor dysfunction (situational)
- Emotional “fall out” from vulvovaginal condition
- Unprotected sex for two years, without pregnancy
Plan:
Testing sent or ordered: Yeast culture; results: negative;
Herpes titer for type 1 and 2; results: positive for both type 1 and type 2.
Education: Discussed and handouts given on general vulvar care, avoidance of irritants, sexuality in long-term relationships, fear of intercourse from experience of having pain, pelvic floor dysfunction as a result of that fear. Also discussed getting fertility evaluation, ovulation testing kit.
Handout given on pelvic floor physical therapy.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days.
Phone call with lab results: the patient was called and informed of her herpes titer result. She was very upset and did not believe the diagnosis. She said she knew that herpes always involved blisters and she had never had blisters. She was told that herpes outbreaks often start with itching and irritation; the blisters, when they form, collapse very quickly and pain is not noticed until then. She understood that her symptoms had started four years before, before her current relationship.
Treatment: Acyclovir 400 mg orally twice a day was advised. This is Category B for pregnancy. The patient was advised to use Preseed lubricant for intercourse. She was offered pelvic floor physical therapy, but she declined it. She did accept referral for fertility work up.
Return visit findings:
Two months later:
The patient reported no flares in symptoms. She was in the middle of fertility testing and treatment. She had not told her boyfriend about the herpes diagnosis. She was still saying that herpes was impossible, but also asking how to tell him. She had worked on eliminating possible irritants: Always brand pads and liners and frequent wet wipes and on “soak and seal,” using plain Vaseline for moisturizing, and intercourse was more comfortable.
TEACHING POINTS:
- Herpes simplex is extremely common and does not always present in a “classical” way. The virus can first appear in one area and can migrate to new sites in the genital area. Herpes can present as fissures rather than ulcers, and can cause discomfort and pain without any outbreak at all.
- Vulvovaginal conditions can be devastating for individuals and for relationships.