#16: Burning and itching
Age, G/P, relationship status, occupation: 59 year old, G2P2, married RN
Menstrual status: Postmenopausal
Contraceptive method: none
Sexuality status: male partner, sexually active with spouse of 40 years until two months ago.
Chief complaint: vulvar burning and itching
Symptoms (HPI: history of present illness): Vulvar burning and itching started approximately 5 years prior to this visit, about the time she became menopausal. Her burning was significant, sometimes reaching 7-8/10. She had biopsies and cultures done, and states that all of her workup was negative. She was given a trial of clobetasol, but this was of no value to her. She was diagnosed with vulvodynia. She took amitripyline in a low dose and thought it helped to a slight degree, but she could not tolerate the side effects. Over the years, her symptoms worsened. Nine months prior to this visit, another biopsy was done that was non-specific. Six months prior to this visit, she had a biopsy in the vulvar vestibule at 5 o’clock that showed epidermis with hyperkeratosis, parakeratosis, and a dense, band-like, mononuclear, cellular infiltrate in the dermis, indicative of possible lichenoid dermatitis, but without the degenerative changes in the base of the epithelial layer which would be expected for a lichenoid disease. There was no hyalin change in the dermal connective tissue, which would be expected in lichen sclerosus.
The patient was then given clobetasol again on a three times daily basis, and gradually, over the months, her symptoms improved to some degree. She still has virtually constant burning that she rates at about 3/10 and then after she has been on her feet and worked for a period of time, her symptoms can go to 7-8 again. She uses Vagicaine on a regular basis to help with burning. She has been able to have intercourse up until the past two months without difficulty.
Lifestyle issues: uses Vagisil and Vagicaine
History and review of systems:
- Vulvovaginal history: denies
- GYN history: uterine prolapse with pessary use for ten years. She inserts, removes, and cleans it herself, three times weekly. Pap smears normal.
- Past and current medical conditions: hypothyroidism, Crohn disease, sinus headaches, SVT (supraventricular tachycardia) related to over the counter antihistamine use, not currently a factor.
- Past surgical history: no history of surgery
- Review of associated systems:
- Urinary: denies
- GI: history of diarrhea and Crohn disease diagnosed at menopause. Controlled with Entocort (budesonide).
- Musculoskeletal: history of sciatica
- Dermatological: denies
- Review of other systems: negative
- Social history: never used alcohol, smokes one half pack per day, never used recreational drug, no exercise outside of work (walking in her job)
Medications:
- Levothyroxine 50 mcg orally daily
- Atenolol 25 mg orally daily
- Budesonide (Entocort EC) 9 mg orally daily
- Calcium citrate 2 tabs orally daily
- Vitamin D3, 2,000 units orally daily
- Multivitamin 1orally, daily
- Omega-3 fatty acids/fish oil 300/1,000 mg orally daily
Allergies:
- Sulfa (Sulfonamide Antibiotics)
KEY POINTS FROM THE HISTORY:
- Immediately obvious is the use of a potent steroid (budesonide) for Crohn disease, making her at risk for Candida albicans or herpes from local immune suppression.
- Candida may have started the initial itching and burning. Topical clobetasol added to the problem and then her use of OTC products with benzocaine, a potent irritant, put her symptoms out of control.
- The use of the pessary may also have contributed to the perpetuation of yeast.
- Her biopsy showed lichenoid inflammation that can be associated with lichen sclerosus (but characteristic hyalinization was not seen), with lichen planus (but degenerative changes in the basal epithelial cell layer that would be expected were not seen), or with a drug reaction . She was using benzocaines that may have produced the lichenoid findings.
- Hypothyrodism is associated with lichen sclerosus.
Non-genital exam:
BMI: 20.4 kg/(m^2); vital signs within normal range
GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear, without lesions. NAILS: normal. NECK: supple, without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Exam: well tolerated.
Mons pubis: erythematous.
Groin: normal skin color and texture
Labia majora: erythematous in contactant pattern (mottled, confluent, with whitening) from anterior commissure to perineum .
Perineum: erythematous.
Anus: normal skin color and texture.
Bulbocavernosus reflex and anal wink present.
Labia minora: absent from 2:00-10:00, erythematous
Prepuce: normal and mobile.
Clitoris: visible.
Interlabial folds: erythematous
Vestibule: mildly tender, mottled with erythematous patches and whitened patches
Urethral meatus: normal size, normal location, no masses.
Vagina: atrophic, erythematous, and inflamed. Pessary removed for adequate exam. Walls flaccid; Discharge: copious and yellow.
Pelvic Floor: there is no hypertonicity.
Cervix: no lesions, no cervical motion tenderness, multiparous appearance and prolapsed.
Uterus: midline, mobile, smooth, non-tender, not enlarged.
Adnexa: not enlarged, no masses felt, non-tender.
Rectal: not indicated.

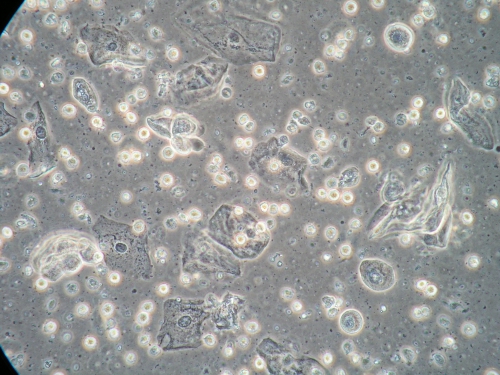
Microscopy:
Vaginal pH: 7.0
Wet prep: normal epithelial cells, parabasal cells: 30%, no yeast forms seen, sheets of WBCs per epithelial cell and absent lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM THE EXAM:
- It is not possible to say whether absence of labia minora from 2-10 o’clock represents pathology such as lichen sclerosus or lichen planus or whether this is her normal architecture.
- The synechial bridge at the base of the vaginal opening suggests pathology.
- Erythema could represent a dermatosis, Candida albicans, or contact dermatitis from benzocaine topicals.
- The elevated pH shows probable lack of estrogen. The presence of parabasal cells and lack of lactobacilli can represent either atrophy or an inflammatory process. The sheets of white blood cells show inflammation.
PRELIMINARY DIAGNOSIS:
- Biopsy proven lichenoid vulvitis, possible lichen planus
- Benzocaine contact dermatitis
- Uterine prolapse with pessary management
- Profuse vaginal discharge with abnormalities in the pH and wet prep: R/O Candida albicans, atrophy, inflammatory vaginitis related to Crohn disease or lichen planus, pessary use, atrophy
- Crohn disease, in control with Entocort
- Hypothyroidism
- Resolved SVT from overuse of antihistamines
Plan:
Testing sent or ordered: yeast culture, Result: positive for C. Albicans and bacterial culture, Result: negative (only normal skin flora found)
Education: stop benzocaine, avoid irritants, use gentle care; handouts given on lichen planus, irritant dermatitis, the use of steroids in vulvar care, vaginal atrophy, and general vulvar care; conditions discussed
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days. If something needed to soothe the skin, outside of Vaseline, to use zinc oxide.
Treatment: IM triamcinolone 60 mg depot injection
Return visit findings:
One month later:
The patient had been called one week after the initial visit with positive yeast culture results: (C. Albicans). She had been asked to take 150 mg of fluconazole in two doses, 3 days apart. She had not been able to find zinc oxide but used Desitin with 40% zinc oxide in it with improvement.
At the first follow-up visit she was “90% better” and she became entirely comfortable subsequently. She is maintained on clobetasol once weekly. Since lichen planus may regress, taper of clobetasol will be attempted in the future.
Her yeast culture was positive for Candida albicans at the initial visit and she was treated with fluconazole 150 mg for two doses, 72 hours apart.
Follow up visits:
Her yeast culture was still positive at the follow up visit and has remained positive. She has had sensitivity testing with an MIC of 2 for fluconazole, indicating sensitivity. Positive culture persisted on fluconazole 200 mg twice weekly and continued with a change to itraconazole 200 mg twice weekly (MIC 0.25). She is not symptomatic with these positive cultures; it is possible that the budesonide may be perpetuating the Candida. Since she has no symptoms, she is maintained on itraconazole 200 mg twice weekly with LFT monitoring.
The patient was able to resume intercourse and remain comfortable with it without treatment for atrophy.
TEACHING POINTS:
- With a number of possible causes of symptoms, it is important to follow logical rule outs. For the vulva, first eliminate any possible irritant and provide gentle care. Check with bacterial skin culture for staph and strep on the skin and treat if necessary. If using an antibiotic, always cover for yeast. Then reevaluate.
- For the vagina, always check a yeast culture first, and rule out atrophy before diagnosing any other form of inflammation. Then re-evaluate.
- In this case, sudden withdrawal of chronic benzocaines can lead to painful rebound. IM triamcinolone was used to bridge the gap and to cover for possible lichen planus until she could use topical treatments.
- The persistence of C. Albicans in this patient was unusual. She had multiple factors that contributed to this: treatment for Crohn disease, the use of topical steroids, and the use of the pessary. In this situation, she accommodated to the constant presence of yeast.