#1: Itching
Age, G/P, relationship status, occupation: 43 year old G3 P3 (all vaginal births), married, at home mom.
Menstrual status: Getting monthly periods
Contraceptive method: Condoms
Sexuality status: Male partner, not currently sexually active due to vulvar problem
Chief Complaint: Worsening vulvovaginal itching
Symptoms (HPI: history of present illness): For the last six months, the patient has been having increasing bouts of itching in the genital area. She has tried topical Monistat and changing soaps and detergents. She has been treated with oral fluconazole for yeast, but symptoms recurred. She was then treated for bacterial vaginosis with Metronidazole. This made her worse so she was put on weekly fluconazole. The last time she took it was three days ago. The itching is driving her crazy. She has stopped having sex with her husband because she worries that she has something contagious and will give it to him. The itching seems worse at night. The only thing that helps is putting bags of frozen peas on the area.
Lifestyle issues:
Loves to exercise at the gym; wears daily panty liners so that she does not ruin her underwear.
History:
- Vulvovaginal history: occasional yeast infections in the past
- GYN history: No abnormal Paps
- Past and current medical conditions: Migraines
- Past surgical history: No history of surgery
- Social history: No smoking, no alcohol, no drugs, exercises 5 days a week at the gym
- Review of associated systems:
- Urinary: sometimes has burning when she urinates; denies frequency or urgency, leakage of urine
- GI: Has episodic constipation and then loose stools
- Musculoskeletal: None
- Dermatological: None
- Review of other systems: headaches now and then
KEY POINTS FROM THE HISTORY:
- Extensive itching despite treatment for yeast is pointing to a dermatosis such as lichen sclerosus or to lichen simplex chronicus, eczematous dermatitis, or an irritant reaction.
- She does exercise a lot and she wears daily panty liners; the history is otherwise non-contributory.
Non-genital exam:
BMI: 20.57 kg/(m^2); vital signs within normal range.
GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam with symptom mapping:
Exam: well tolerated
Mons pubis: normal, non-tender.
Groin: normal skin color and texture
Labia majora: normal skin color and texture and normal anatomy.
Perineum: dark pink, lichenified. Itching is present.
Anus: dark pink, lichenified. Itching is present.
Bulbocavernosus reflex and anal wink present.
Labia minora: normal architecture bilaterally, whitened skin with fine excoriations; itching is present.
Prepuce: normal and mobile. Pink, with whitened area surrounding.
Clitoris: visible. Normal in color and texture.
Interlabial folds: whitened, increased skin markings; itching is present with Q-tip touch.
Vestibule: non-tender to q-tip test, normal skin color and texture; no itching.
Urethral meatus: normal size, normal location, no masses.
Vagina: well estrogenized, not inflamed and non-tender; Discharge: normal and scant.
Pelvic Floor: no hypertonicity on exam
Cervix: no lesions, no cervical motion tenderness.
Uterus: midline, mobile, smooth, non-tender, not enlarged.
Adnexa: not enlarged, no masses felt, non-tender.
Rectal: not indicated.

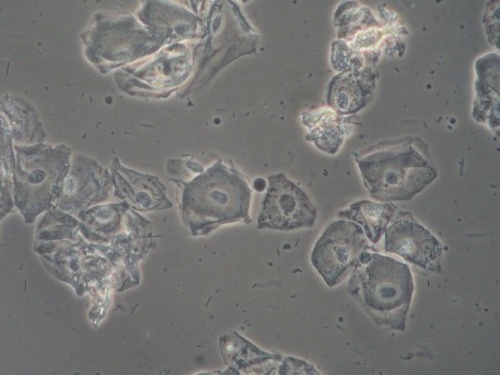
Microscopy:
Vaginal pH: 4.0
Wet prep: normal; one WBC per epithelial cell, no clue cells, no parabasal cells, no pathogens, normal lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM THE EXAM:
- In the setting of normal anatomy, that is, no architectural changes that would lead to suspicion of dermatosis, the lichenification and whitening of the skin, particularly with broken hairs and excoriations, point to lichen simplex chronicus (histologically the same as eczematous dermatitis).
PRELIMINARY DIAGNOSIS:
- Lichen simplex chronicus related to probable history of yeast, though none apparent today, daily panty liner use, frequent exercise in lycra clothing.
Plan:
Testing sent or ordered: Yeast culture Results: negative
Education: Discussion and handouts on lichen simplex chronicus, with emphasis on the need to stop scratching. Discussed the importance of eliminating irritants: panty liners, tight clothing, lycra that does not breathe although it stretches
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days.
Treatment:
1) Start applying a thin film of betamethasone valerate 0.1% ointment twice a day for 14 days, then once a day every other day for 14 days to the itchy areas.
2) Continue weekly fluconazole 150 mg orally for another two months
3) Stop scratching! Take an antihistamine at night to reduce itching and enhance sleep: Atarax 10-20 mg orally at bedtime for a few nights, at least.
4) Use topical Lidocaine 5% if the itching is bad. In between treating with steroid ointment, use topical petroleum jelly as an emollient.
5) Return in one month for follow up.
Return visit findings:
One month later:
Yeast culture from the first visit was negative. Patient was much better. She was informed that this condition may recur if she allows contact with irritants (including tight clothing) or gets recurrent yeast.
Assessment: Lichen simplex chronicus in good control
Plan: Continue warm soaks and petroleum jelly for comfort. Stop weekly Fluconazole. To call and come in if she gets itching again for correct diagnosis and treatment.
TEACHING POINTS:
- It is important to correctly diagnosis yeast and bacterial vaginosis. If pseudohyphae are clearly seen under the microscope, one can assume Candida albicans and treat accordingly. Budding spores can be either albicans or non-albicans yeast. Doing a culture at each visit is helpful.
- Yeast is missed under the microscope 40% of the time. Bacterial vaginosis is easily identified with KOH and microscopy: Amsel’s criteria are still relevant: positive whiff, the presence of clue cells, the absence of white blood cells, the absence of lactobacilli, and an elevated pH. Treating for BV may cause a yeast infection.
- Not everything is yeast or BV!