#13: Dyspareunia
Age, G/P, relationship status, occupation: 54 year old G0, married, advocate for legislation, stable relationship
Menstrual status: post-menopausal
Contraceptive method: N/A
Sexuality status: Male partner; unable to have vaginal intercourse for the past four years. She denied prior history of dyspareunia and had no history of abuse. She and her husband had had “some relationship issues” but they had “worked things out.”
Chief complaint: dyspareunia
Symptoms (HPI: history of present illness): She was having comfortable intercourse with her husband until about 4 years ago. She then noticed increasing discomfort with sitting and riding a bicycle, resulting in an uncomfortable pressure sensation. Later, she noted fissuring at the introitus making intercourse so painful that she had stopped. She has been using vaginal estrogen for the past six years, with eventual remission of her unprovoked symptoms. She was started on amitriptyline five years ago, is up to 20mg orally at bedtime, tolerating that moderately well. She would like to be able to have comfortable sex again.
Lifestyle issues: active, enjoys biking
History and review of symptoms:
Vulvovaginal history: yeast infections in the past, chlamydia at age 20; history of genital herpes, currently quiescent; she denies history of genital trauma or abuse.
Gynecologic history: negative; no abnormal Pap smears.
- Past and current medical conditions: pneumonia six years ago, osteoporosis
- Past surgical history: benign breast biopsy years ago x 2
- Review of associated systems:
- Urinary: negative
- GI: negative
- Musculoskeletal: knee injury six years ago, had physical therapy and rehabilitation
- Dermatological: negative
- Other review of systems: negative
Social history; does not smoke, two drinks a week, no recreational drugs, exercises 4 hours weekly
Medications:
- Amitriptyline 20 mg orally at bedtime
- Fosomax 70 mg orally weekly
- Vagifem 10 mcg vaginally, twice weekly
- Lidocaine 5% topically up to five times a day, as needed, in vulvar area
Allergies:
- Sulfa
- Erythromycin base
KEY POINTS FROM THE HISTORY:
- Dyspareunia in menopausal woman has been helped by local estrogen.
- Biking may be an irritant but is unlikely to be causative.
- The history of relationship issues needs to be kept in mind.
Non-genital exam:
BMI: 23.5 kg/(m^2). Vital signs within normal range.
GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital Exam and symptom mapping:
Exam: well tolerated.
Groin: normal skin color and texture
Mons pubis: normal, non-tender. Anterior commissure: normal skin color and texture and normal anatomy.
Groin: normal skin color and texture and normal anatomy.
Labia majora: normal skin color and texture and normal anatomy.
Perineum: normal skin color and texture and normal anatomy.
Anus: normal skin color and texture and normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: normal skin color and texture, flattened posteriorly bilaterally
Prepuce: mobile
Clitoris: visible.
Interlabial folds: normal skin color and texture and normal anatomy
Vestibule: diffusely tender to q-tip touch test, fiery, bright red glazed patches at 3-9:00.
Urethral meatus: normal size, normal location, no masses, no tenderness.
Vagina: not inflamed and non-tender; Discharge: scant.
Pelvic Floor: there is no hypertonicity.
Cervix: no lesions, no cervical motion tenderness.
Uterus: midline, mobile, smooth, non-tender, not enlarged.
Adnexa: not enlarged, no masses felt, non-tender.
Rectal: not indicated.

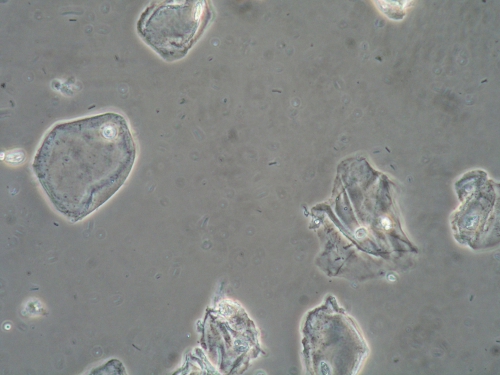
Microscopy:
Vaginal pH: 4.0
Wet prep: normal epithelial cells, one WBC per epithelial cell, no parabasal cells, no clue cells, no pathogens, normal lactobacilli, normal.
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM THE EXAM:
- Architectural changes are characteristic of dermatoses. In this case, the anatomy looks normal, although the labia minora are flattened posteriorly bilaterally.
- The fiery, red, glazed patches in the vestibule, with or without white reticulations, are characteristic of lichen planus, especially in the case of a well-estrogenized vagina.
- Yeast infection, of course, must be ruled out.
PRELIMINARY DIAGNOSIS:
- Vaginal atrophy in good control
- Probable lichen planus
Treatment Plan:
Testing sent or ordered: vulvar biopsy, yeast culture Results: Biopsy: vulvitis circumscripta plasmacellularis (plasma cell vulvitis); Yeast culture: negative.
Education: Handouts given on lichen planus, general vulvar care, the use of steroid ointments in vulvovaginal disease. Possible condition discussed, pending biopsy result.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days.
Treatment: clobetasol 0.05% ointment applied in a thin film, morning and night for eight weeks
Maintenance of adequate local estrogen: continue Vagifem 10 mcg vaginally, twice weekly
Return visit findings:
Two months later:
Biopsy showed vulvitis circumscripta plasmacellularis (also known as plasma cell vulvitis). She had been called with this result and started on topical clobetasol 0.05%, applied in a thin film twice a day for 30 days, then once a day for 30 days. She improved to some degree with clobetasol but could not have intercourse.
She was switched to Protopic 0.03% ointment, a thin film nightly on top of the clobetasol (to prevent burning from the Protopic) and she was asked to continue adequate local estrogen with Vagifem 10 mcg vaginally, twice weekly.
Two months later:
Treatments brought her skin into control after another, but dyspareunia persisted. Pelvic floor hypertonicity had developed.
She was sent for physical therapy to the pelvic floor. She was asked to use Protopic alone, which caused her no burning, plus her Vagifem.
Nine months later:
With physical therapy combined with ongoing local estrogen and Protopic, she could accommodate three fingers, with manipulation, but was still unable to have intercourse. Her skin was clear. She was weaned off of the Protopic.
Four years later:
She was referred for sexual therapy. Underlying relationship issues were identified and treated, leading to successful intercourse after a total of four years of treatment. She continues adequate local estrogen only.
TEACHING POINTS:
- This woman had an epithelial disorder, postmenopausal atrophy, and pelvic floor dysfunction that all needed management.
- Protopic may cause a severe burning sensation in some women. It is also very expensive, often not covered by insurance. Doing the paperwork for prior authorization with the insurance company can sometimes yield coverage. Obtaining tiny samples for trial application can be helpful in testing the medication before patients try to obtain it on their own.
- Plasma cell vulvitis can be hard to treat. Steroid ointments may or may not help, but are appropriate for treatment. In the case of this patient, biopsy was key to diagnosis.
- Despite adequate treatment of the epithelium, use of local estrogen, and pelvic floor physical therapy, dyspareunia persisted.
- Relationship and intimacy issues that she had previously denied were identified and treated by a sexual therapist.