#3: Itching, irritation, pain, dyspareunia
Age, G/P, relationship status, occupation: 29 year old, G0, married 4 years, marketing and sales manager.
Menstrual status: regular menses
Contraceptive method: OCP
Sexuality status: Male partner; no prior history of dyspareunia. Vaginal intercourse currently impossible because of pain and fissuring. There is pain with sexual touch on the vulva and pain with oral sex. No history of genital injury, sexual assault, sexual abuse.
Chief complaint: vulvar itching and irritation, pain and dyspareunia
Symptoms (HPI: history of present illness): Two years ago she had a lesion on the vulva that was treated with liquid nitrogen ten times before the lesion resolved. No pathology available. Subsequently, she developed itching, dyspareunia and vaginal spotting. Endometriosis was suspected. No records are available of work-up or months of different medications and treatments by patient report.
One year before her initial visit with us, she underwent evaluation under anesthesia, laparoscopic left ovarian cystectomy, chromopertubation, biopsy of left pelvic sidewall, hysteroscopy, and injection of the vestibule with 10 cc bupivacaine 0.25% with epinephrine.
Evaluation under anesthesia revealed normal uterus, normal adnexa. External genitalia showed inflamed, erythematous vestibule and perineum with a 1-2 cm fissure on the perineum.
Laparoscopy revealed a 3 cm left simple ovarian cyst that was removed intact from the ovary. The rest of the pelvic anatomy was entirely normal. Biopsy showed no abnormality.
She was diagnosed with vulvodynia and referred for pelvic floor physical therapy. After six months, she had made some progress but was still having severe intromission pain and was generally unable to allow penetration.
Lifestyle issues: she has correctly eliminated contact irritants except for spandex worn for workouts 5-6 hours a week.
History and review of systems:
- Vulvovaginal history: history of yeast infection and genital warts/HPV
- GYN history: history of ovarian cyst (see HPI) and pelvic pain. Being followed for abnormal Pap smear with persistent HPV.
- Past and current medical conditions: migraines
- Past surgical history: laparoscopy, hysteroscopy
- Review of associated systems:
- Urinary: history of urinary frequency, but drinks large amounts of water
- GI: History of constipation, controlled with diet.
- Musculoskeletal: History of chronic low back pain
- Dermatological: History of itching, and bad eczema of hands, feet, and face. Mother with eczema and father with eczema and psoriasis
- Review of other systems: childhood asthma, migraines
- Social history: no tobacco; alcohol 3 drinks a week, runs, does yoga and weights 5-6 hours a week.
Medications:
- Gabapentin 100 mg orally daily, for sleep
- Nortrel OCP
Allergies:
- Amoxicillin
KEY POINTS FROM THE HISTORY:
- This young woman had normal sexual function until two years ago. The first consideration is fissuring with primary causes of Candida, herpes and dermatitis needing to be worked up.
- Patient gives a personal and family history of dermatitis.
- It is unclear what lesion on vulva was treated but repeated cryotherapy would not be helpful to an atopic person with sensitive skin.
- Pain on penetration that would be present with chronically fissured, irritated vulva would account for pelvic floor hypertonicity. She is already in therapy for this, but not moving ahead, because underlying causes have not been addressed properly yet.
Non-genital exam:
BMI: 20.37 kg/(m^2); vital signs within normal range.
GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Exam: well tolerated
Mons pubis: normal, non-tender.
Groin: clear; normal skin color and texture
Labia majora: erythematous with sensation of irritation
Perineum: dark pink, slightly lichenified, with scarring from old fissures, some scaling posteriorly.
Anus: erythematous anteriorly, below perineum.
Bulbocavernosus reflex and anal wink present.
Labia minora: flattened posteriorly on the right side from 3-6, slightly puffy, erythematous; slightly itchy.
Prepuce: normal and mobile, erythematous.
Clitoris: visible, erythematous.
Interlabial folds: erythematous
Vestibule: diffusely tender to q-tip touch test at a level of 8/10, erythematous
Urethral meatus: normal size, normal location, no masses.
Vagina: well estrogenized, not inflamed and non-tender; Discharge: scant and white.
Pelvic Floor: hypertonicity on exam, but able to relax muscles with “pelvic floor drop” exercise
Cervix: no lesions, no cervical motion tenderness.
Uterus: midline, mobile, smooth, non-tender, not enlarged.
Adnexa: not enlarged, no masses felt, non-tender.
Rectal: not indicated.


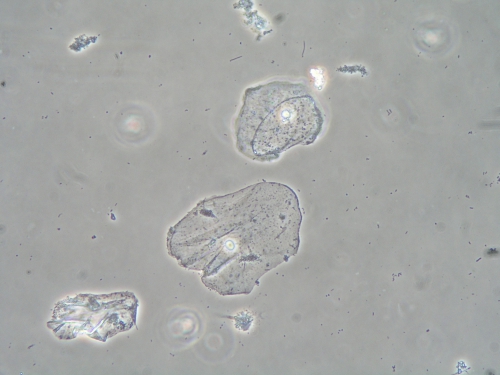
Microscopy:
Vaginal pH: 4.0
Wet prep: normal epithelial cells; one WBC per epithelial cell, no clue cells, no parabasal cells, no pathogens, normal lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
PRELIMINARY DIAGNOSIS:
- Vulvar inflammation and fissuring with cause unclear: yeast infection despite negative wet prep, lichen simplex chronicus related to history of atopy/eczema?
- Dyspareunia and pelvic floor dysfunction, probably secondary to skin conditions
- Possible Candida and possible herpes simplex
Plan:
Testing sent or ordered: yeast culture, herpes serology titers (type 1 and 2) for IgG. Result: yeast culture positive for C. Albicans, herpes titers negative.
Education: Handouts given on general vulvar care and on lichen simplex chronicus (because this condition most closely resembled what had happened to the patient’s skin) and how to treat it.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days.
Treatment: Check yeast culture and suppress if positive. Check herpes titers: IgG for type 1 and 2 and suppress if positive. Review irritants and allergens, and advise gentle vulvar care. Vulvar biopsy offered and declined.
If yeast culture negative, begin 5 minute daily soaks followed by betamethasone valerate 0.1% ointment in a thin film, once a day for 30 days and then once a day, Monday, Wednesday, and Friday. Continue the gabapentin orally at bedtime for sleep. Continue physical therapy to the pelvic floor. Try lidocaine 5% ointment applied to the vaginal opening for 15 minutes and then wiped off and replaced with a lubricant prior to intercourse.
Since yeast culture was positive for C. Albicans, she was treated with fluconazole 150 mg orally twice a week for two weeks. Herpes serology was negative. She began the betamethasone valerate 0.1%, as directed.
Return visit findings:
Two months later: She felt that betamethasone and fluconazole both helped but she continued to itch at a level of 5/10. Lidocaine, even applied 15 minutes ahead and wiped off before intercourse, numbed her husband. She continued to work with physical therapy, but intercourse was still painful. On examination, there was resolution of erythema and fissuring. Skin appeared normal. She was asked to lower betamethasone valerate to twice weekly and to start suppression of Candida with weekly fluconazole 150 mg. She planned to continue her physical therapy to the pelvic floor.
Yeast culture was negative at that visit. Her physical therapist suggested diazepam vaginal suppositories 10 mg nightly to relax the pelvic floor muscles and these were started.
Six months later: She reported that she was comfortable and free of itching. She was able to have sex without pain with the exception of a trigger point identified at 3 o’clock in the vestibule. A urogynecologist injected the trigger point with lidocaine and cortisone for resolution of her pain and she was discharged from physical therapy. She stopped the vaginal Valium. She continues on gentle care and irritant avoidance, oral fluconazole 150 mg suppression weekly for six more months, betamethasone valerate 0.1% as needed.
TEACHING POINTS:
- Vaginal yeast culture is always the gold standard to rule out Candida albicans that was present without classical findings on wet prep in this patient.
- Weekly yeast suppression in the effort to eliminate Candida is equally important to control itching and irritation in an atopic patient.
- With known causes of vulvar pain: eczema and recurrent yeast, leading to painful intercourse and pelvic floor muscle hypertonicity in response to pain, vulvodynia is not the correct diagnosis. If dyspareunia had persisted after the skin was totally healed, vulvodynia secondary to the trauma of her skin condition would have to be considered.