#17: Pain with attempts at intercourse
Age, G/P, relationship status, occupation: 25 year old, G0; single but living with her partner of three years; works for a PR firm
Menstrual status: regular menses
Contraceptive method: OCP: Tri-previfem
Sexuality status: Unable to have intercourse
Chief complaint: Pain with attempts at intercourse
Symptoms (HPI: history of present illness): The patient says that she had a problem, as a teenager, using tampons. She has never been able to get them in. Then, when she first tried to have intercourse with her boyfriend two and a half years ago, she found it impossible. They have tried a few times since then. He is able to insert a finger into her vagina, but only so far; then he “hits a wall.” She finds even the insertion of one finger to be tight and painful. With each failure, she feels more and more anxiety and stress. She says that the problem seems to be getting worse instead of better. She has never been able to tolerate a pelvic exam or speculum exam, either.
Menarche was at age 12 and periods have been regular. She has been on the OCP for a while. Two years ago, she started to have persistent pelvic pain and was diagnosed, by ultrasound, with bilateral ovarian cysts. She had a laparoscopic procedure done to remove the cysts. This was completely successful and resulted in resolution of her pain, but it was noted that she had endometriosis. Her doctor simply advised her to stay on the OCP. She did not tell her whether or not the endometriosis had been treated.
No pain while doing any other activities. No itching.
Treatments tried: the patient has gone to a gynecologist for advice and it was at that visit, that the ovarian cysts were identified. She and her boyfriend thought they could work the painful intercourse out together, but now she is worried that they cannot.
Lifestyle issues: Uses Tide detergent. No daily panty liners.
History and review of systems:
- Vulvovaginal history: diagnosed with both yeast and bacterial vaginosis.
- GYN history: No Paps done, ever. Was diagnosed with endometriosis when she had laparoscopy for bilateral ovarian cysts with cystectomies.
- Past and current medical conditions: endometriosis, pelvic pain, eczema
- Past surgical history: Laparoscopy, cystectomy
- Review of associated systems:
- Urinary: No symptoms
- GI: reflux
- Musculoskeletal: No symptoms
- Dermatological: eczema
- Review of other systems: negative
- Social history: non-smoker; drinks 2-3 drinks a week, no recreational drugs, no regular exercise
Medications:
- None; has received Gardasil
Allergies:
- Amoxicillin
KEY POINTS FROM HISTORY:
- Psychogenic vaginismus may be suspected, but exam must be done to rule out a physical reason for the pain.
- She has eczema but is not complaining at all about itching.
Non-genital exam:
BMI 19.85 kg/m2
General: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
The exam is tolerated with discomfort.
Mons pubis: normal, non-tender. Anterior commissure: normal skin color and texture and normal anatomy
Labia majora: normal anatomy and uniformly erythematous. The pt is completely comfortable with q-tip touch in the labia majora. This may be her natural coloration.
Perineum: normal skin color and texture and normal anatomy.
Anus: normal skin color and texture and normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: flattened posteriorly, right side between 6 and 9 o’clock and flattened posteriorly, left side between 4 and 6 o’clock, normal skin color and texture
Prepuce: normal and mobile.
Clitoris: visible.
Interlabial folds: normal skin color and texture
Vestibule: The vestibule is non-tender to q-tip test except in close to the hymenal ring. The patient SAYS there is pain, but it’s as if she has to really think about it. Normal skin color and texture; she was able to allow passage of a Q-tip into the vagina for the pH and wet prep.
Urinary meatus: normal, normal size, normal location.
Vagina: well estrogenized; Discharge: normal and white.
Pelvic Floor: hypertonicity is present.
Cervix: exam deferred due to patient guarding, pain.
Uterus: deferred for pain.
Adnexa: deferred for pain.
Rectal: not indicated.

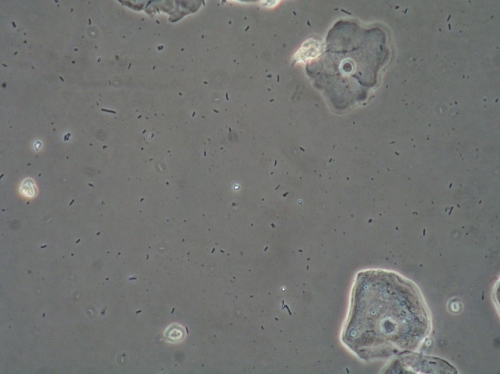
Microscopy:
Vaginal pH: 4.0
Wet prep: normal; one WBC per epithelial cell, no clue cells, no parabasal cells, no pathogens, normal lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM EXAM:
- The normalcy of the exam, including a lack of obvious pain with q-tip touch, points to a diagnosis of pelvic floor dysfunction/vaginismus.
- There was slight pain at 6:00 at the hymenal ring, leading to an alternative possible diagnosis of vulvodynia.
- The labia majora are erythematous, but she has no complaints in that area.
PRELIMINARY DIAGNOSIS:
- Pelvic floor dysfunction/vaginismus
- Possible vulvodynia
Plan:
No tests were sent. With one finger in the vagina (with the pt’s permission), I attempted to teach her how to do pelvic floor drop: (“squeeze the muscles in the back as if you were trying to stop yourself from passing gas and urine. Hold the squeeze, then relax it, letting the muscles drop down. Then do a small push outward as would happen if you coughed.”) The patient’s muscles did not relax with this maneuver. I could feel her doing the squeeze, but relaxation did not reduce the hypertonicity.
We had a discussion about possible causes for pelvic floor hypertonicity from her past: sometimes toilet training or having issues with retaining urine or stool can cause chronic muscle hypertonicity. She does not remember anything like this that could account for it. We did not talk about possible cultural or social issues that might contribute.
I told her that I could not tell absolutely whether or not the hymen was still present. The opening did allow one finger up to the fleshy joint near my hand. There was no rigidity to the hymenal ring. The rigid tissue was in the muscle behind the ring.
Education: Handouts were given on the following topics: The V Book, Vaginal Microscopy, Vulvodynia, My partner has vulvodynia; Pelvic floor dysfunction, the PT list, and the pamphlet: Why sex hurts. We discussed the specifics of avoiding irritants and what they might be, including thongs, tight jeans, daily panty liners, underwear to bed, wet wipes, etc.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days.
Treatment: The patient was referred for pelvic floor physical therapy.
Advised to try lidocaine 5% prior to physical therapy or intercourse as follows: Once you feel ready to try intercourse, you can try this: Apply a generous amount of the lidocaine 5% ointment to the tender tissues at the opening of your vagina and leave it on for 10 to 15 minutes before sex. Avoid getting it on your clitoris. Wipe the ointment off just before having sex. The numbing effect of this topical anesthetic should help reduce your sexual pain. Do not be alarmed if the lidocaine stings when you first apply it. This will resolve within 45 seconds and then the skin will numb. Use a lubricant if you wish.
Follow up phone calls:
Call from patient two months later: still having pain with touch. Advised by the physical therapist to try vaginal Valium 5 mg and she wanted to try it. Advised to score the tab, run it quickly under water, then insert into vagina at bedtime. Pt warned of possible sedation; advised to try it initially when she has no obligations the next morning that require her to be alert, e.g. driving, working, etc, in case she feels sedated. If tolerated, pt advised to use nightly x 30 d.
Call from patient one month after that:
The patient reported that she had been making great strides with physical therapy. She had started having intercourse, which she was previously unable to do. She had tried going without the vaginal valium but found she was not ready to stop it yet. Requested a refill. Warned about the possibility of dependency.
No further contact with patient six months later.
TEACHING POINTS:
- Although the patient has come for the exam, wanting to be “fixed,” she may not be able to go through with it because of fear of pain.
- It is important to be very patient and allow the patient to say when she is ready to be touched. Every time the patient’s point of view is respected, she will trust the clinician a little more, finally allowing enough touch to inspect the anatomy, color and texture of the skin, and do a Q-tip touch test. She may be able to allow gentle passage of a q-tip for pH and wet prep. She may need to insert that herself if fear of pain is too great.
- Sometimes, patients cannot bring themselves to go to another practitioner (e.g. a physical therapist) with this very private problem. Having come to you, however, by the end of the first visit, they may feel enough trust to allow evaluation of the pelvic floor and the teaching of the pelvic floor drop technique. If you feel comfortable with it, the smallest size dilators (no more than two) may be offered to the patient to work with on her own. Ideally, she would use the dilator first, with you present. See annotation D and annotation L and the document Pelvic Floor Dysfunction/Vaginismus for more on this.