#18: Burning, itching, fissuring
Age, G/P, relationship status, occupation: 59 year old G2 P2 (both C/S), widowed woman in a new relationship for the last five years; works as office manager.
Menstrual status: Postmenopausal since the age of 46.
Contraceptive method: N/A
Sexuality status: Male partner; sex used to be pleasurable; has not had intercourse for two months because of discomfort
Chief complaint: vulvovaginal burning, itching, and fissuring for the last six months
Symptoms (HPI: history of present illness): The patient feels that her symptoms date back six months or more. She was on vacation. She awoke with a sensation that she scratched herself during the night. Her skin was sore. She self-treated with bacitracin, and her symptoms disappeared, but returned about two months later. This time she was treated for Candida, but the Monistat did not help her. Her physician was unable to find anything and, once again, her symptoms resolved. Subsequent to this, she, again, noted some fissuring of the skin and for this, she was treated for atrophy. When she continued to have splitting, she was given oral Diflucan that she felt was of help. Monistat and topical creams made her miserable to the point that she was up all night. Currently, the skin is better, but she still has soreness and paresthesias in the clitoral area, and the skin will fissure with intercourse. She has not been sexually active for the last two months because of this. Today, she does not have any itching or burning or discomfort, but she feels that the fissures are probably present.
Lifestyle issues: Contactants are not a problem.
History and review of systems:
- Vulvovaginal history: yeast: 1-4 times in her life. She denies any history of genital injury or trauma
- GYN history: remarkable for ovarian cyst in teens, tubal ligation. There is no history of fibroids, endometriosis, or pelvic infection. Pap smears have been abnormal with positive HPV, being followed. She understands that a Pap smear is not done as part of the vulvovaginal evaluation.
- Past and current medical conditions: Hypertension, reflux, hypercholesterolemia; history of blood clot while on OCPs.
- Past surgical history: Appendectomy, tonsillectomy, Cesarean section x 2
- Review of associated systems:
- Urinary: Denies dysuria, frequency, urgency, nocturia, interstitial cystitis, incontinence, frequent bladder or kidney infections, urinary tract surgery.
- GI: Denies constipation, diarrhea, IBS, Crohn’s disease or ulcertive colitis, colon cancer, abdominal pain, rectal fissures, hemorrhoids, rectal bleeding. Has reflux.
- Musculoskeletal: Denies back injury, chronic back pain, arthritis, sciatica, herniated disc, back surgery, fibromyalgia
- Dermatological: History of basal cell ca removed from back
- Review of other systems: Constitutional: negative symptoms, EENT: negative symptoms, Cardiovascular: HTN, occasional irregular heartbeat, no symptoms today, Breasts: negative history or symptoms, Respiratory: history of PE on OCP; no symptoms, Endocrine: negative symptoms, Neurologic: negative symptoms, Psychiatric: negative symptoms
Social history: Alcohol: 6-8 drinks per week; Cigarettes: smoked for years, quit age 38; Drugs: never; Exercise: rarely
Medications:
- Atenolol 25 mg orally , 1 tab twice a day
- Pravastatin 20 mg orally, 1 tab at bedtime
- Omeprazole 20 mg delayed release, 1 cap orally in the morning
- Fish oil 1,200-144 mg-215 mg, 1 capsule orally daily
- Vitamin C 500 mg SR, 1 capsule orally daily
- Vitamin E 400 units, 1 tab orally daily
Allergies:
- Amoxicillin
KEY POINTS FROM HISTORY:
- Persistent itching, irritation, and fissuring, despite adequate treatment for possible yeast points to a dermatosis: eczematous dermatitis, lichen simplex chronicus, or lichen sclerosus or lichen planus.
Non-genital exam:
BP 136/72 | Pulse 62 | Ht 5′ 3″ (1.6 m) | Wt 166 lb (75.297 kg) | LMP Postmenopausal; GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions . NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder
Genital exam and symptom mapping:
Exam: well tolerated.
Mons pubis: normal. Anterior commissure normal.
Labia majora: normal skin color and texture.
Perineum: normal skin color and texture.
Anus: normal skin color and texture.
Bulbocavernosus reflex and anal wink present.
Labia minora: absent 6-9, adherent to interlabial sulcus 3-6, dusky red
Prepuce: scarred to the glans. Fissuring at margins bilaterally, more on left than on right.
Clitoris: barely visible.
Interlabial folds: diminished in width, the skin is whitened, especially on the left side
Vestibule: The vestibule is non-tender to q-tip test, erythematous
Urethra: normal size, normal location, no masses.
Vagina: well estrogenized; Discharge: scant and white.
Pelvic Floor: there is no hypertonicity..
Cervix: no lesions, no cervical motion tenderness, and multiparous appearance.
Uterus: midline, mobile, smooth, non-tender, not enlarged.
Adnexa: not enlarged, no masses felt, non-tender.
Rectal: not indicated.
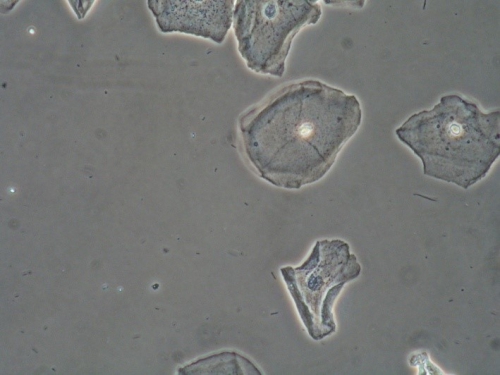
Microscopy performed using a phase contrast microscope shows:
Vaginal pH: 4.0
Wet prep: normal epithelial cells; one WBC per epithelial cell, no clue cells, no parabasal cells, no pathogens, normal lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
With informed consent photo-documentation was done.
Vulvar biopsy- informed consent obtained. EMLA and 1% xylocaine after betadine prep. 3.5 mm punch. AgNO3 for hemostasis. No complications.


KEY POINTS FROM EXAM:
- Architectural changes (adhesion of prepuce to clitoris and diminution or absence of labia minora) are signs of dermatosis.
- Lichen sclerosus is clinically diagnosed when there does not seem to be vaginal or vestibular involvement; if these are present, lichen planus may be the preferred diagnosis.
- Biopsy will usually confirm or refute the diagnosis (but not always).
- pH and wet prep, in this patient, do not show atrophy.
PRELIMINARY DIAGNOSIS:
- Lichen sclerosus with ongoing itching, recurrent fissuring, and subtle architectural changes. Candida may come and go.
- Vaginal atrophy is not an issue.
Plan:
Testing sent or ordered: Yeast culture; Results: negative. Vulvar biopsy; Results: confirms lichen sclerosus.
Education: Given handouts on biopsy after-care, general vulvar care, lichen sclerosus, and use of steroid ointments in vulvar care. Advised to avoid irritants. Advised to do warm water soaks for five minutes, then pat dry gently, prior to using steroid ointment.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water), pat dry, then seal with Vaseline every morning; use steroid ointment every evening, as below.
Treatment: Clobetasol 0.05% ointment applied in a thin film every evening x 30 days, then every other night until seen again in 8-10 weeks.
Return visit findings:
Two months later:
Yeast culture was negative; biopsy confirmed lichen sclerosus.
Patient did well with treatment. She had been able to have comfortable intercourse. However, she was beginning to feel irritation and see redness in the anal area, following some constipation. She had used Clobetasol with relief of symptoms. Also feeling some dryness and itching in the vulvar area.
Exam:
Stable. No change in anatomy. Erythema resolved. Fissuring resolved. Anal area normal in appearance. Vestibular tissue slightly thinned. pH and wet prep normal except for a reduction in lactobacilli.
Asssessment:
Improvement in symptoms related to lichen sclerosus
Lichen sclerosus in good control
Slight vestibular atrophy
Plan:
Cut back on Clobetasol 0.05% to twice a week for ongoing maintenance.
Given prescription for Hydrocortisone 2.5% ointment to use in the anal area sparingly prn.
Advised to use half a pea-sized amount of Estrace cream in the vestibule three times a week. (Patient had been told not to use any estrogen products because of history of blood clot. It was thought that this amount of topical estrogen would not put her at risk.)
Ongoing visit findings:
The patient has been returning for surveillance for the last four years. She has done well, keeping the lichen sclerosus under control with twice weekly Clobetasol. She has been treated a couple of times with oral Diflucan or vaginal Clotrimazole for culture-proven yeast infection. She married her boyfriend. She has continued to produce enough endogenous estrogen to maintain the pH and wet prep in a premenopausal state. At the last couple of visits, she complained of dyspareunia and had been treated for a UTI. She declined vaginal estrogen. Lubricants were recommended, as well as ongoing moisturizing of the vestibular tissue with daily Vaseline. Pelvic floor physical therapy was suggested since the patient admitted that she was tightening up due to fear of pain. Topical Lidocaine 5% was also suggested prior to intercourse.
TEACHING POINTS:
- In this case, the biopsy was very helpful in convincing the patient of the need for ongoing weekly treatment of the vulvar epithelium with steroid ointment.
- Once patients understand their condition, if they are without symptoms, they can space visits out to once every six to twelve months.
- Surveillance is necessary in patients with lichen sclerosus because of the 4-5% risk of squamous cell carcinoma developing.