#11: Burning, itching
Age, G/P, relationship status, occupation: 67 year old G0, single, retired teacher.
Menstrual status: Postmenopausal
Contraceptive method: N/A
Sexuality status: Not sexually active. Did not identify sexual preference. Lives with a woman friend.
Chief complaint: vulvar burning
Symptoms (HPI: history of present illness): The patient experienced increasing, unabating, vulvar itching approximately 2 years ago. Then, one year ago, her PCP noticed whitening of the vulva and referred the patient to a gynecologist who did a biopsy, revealing lichen sclerosus. She was treated initially with clobetasol and then with protopic. While the itching resolved immediately, these medications caused unbearable burning. She was switched to bethamethasone valerate, but daily, constant burning continues. She is looking for recommendations for treatment. She has not been sexually active in many years, and denies any vaginal discharge, STIs, or history of other vaginal problems.
Lifestyle issues: Wears loose, comfortable clothing. No exposure to potential irritants noted in the products she uses.
History and review of systems:
- Vulvovaginal history: no significant history; denies genital trauma or sexual abuse.
- GYN history: No abnormal Pap smears; tiny fibroid on recent U/S.
- Past and current medical conditions: hypercholesterolemia, mild obesity
- Past surgical history: Excision of lipoma on abdomen
- Review of associated systems:
- Urinary: pain with urination, frequent urination, urgency, and occasional leakage of urine, never worked up.
- GI: History of constipation
- Musculoskeletal: History of sciatica
- Dermatological: Negative
- Review of other systems: Negative
- Social history: Non-smoker, rare alcohol, no recreational drugs, very active: hikes and bikes.
Medications:
- Lipitor 10 mg daily
Allergies:
- No known allergies
KEY POINTS FROM THE HISTORY:
- The patient has biopsy-proven lichen sclerosus. This is helpful. You know what you are dealing with. Her clinicians did not know how to manage it when she reported burning.
- Lichen sclerosus does not usually cause burning unless the skin is raw from scratching or something else is going on: yeast, atrophy, irritant or medication reaction, etc.
Non-genital exam:
BMI: 29.44 kg/(m^2). Vital signs within normal range
GENERAL: overweight female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Exam: well tolerated
Groin: normal skin color and texture
Mons pubis: normal.
Labia majora: normal skin color and texture.
Perineum: erythematous with a tender fissure at 6:00; no whitening.
Anus: normal skin color and texture.
Bulbocavernosus reflex and anal wink present.
Labia minora: left side is shortened and absent from 3-6:00 with a stuck-on appearance and whitening. The right side is also shortened and adherent to the interlabial sulcus with whitening. Non-tender.
Prepuce: scarred to the glans and not mobile; scarred to left, upper, labium minus as well.
Clitoris: not visible.
Interlabial folds: whitened anteriorly, no itching or pain.
Vestibule: The vestibule is diffusely tender to Q-tip touch with no lesions; not whitened
Urethral meatus: normal size, no tenderness.
Vagina: Patient tolerated narrow Pederson speculum. Poorly estrogenized, erythematous and tender; Discharge: scant, mucoid
Pelvic Floor: there was no hypertonicity, but there was pain with palpation of the pelvic floor.
Cervix: not seen due to patient discomfort with exam.
Uterus: non-tender, mobile and midline.
Adnexa: not palpable, no masses and non-tender.
Rectal: anal tone normal.

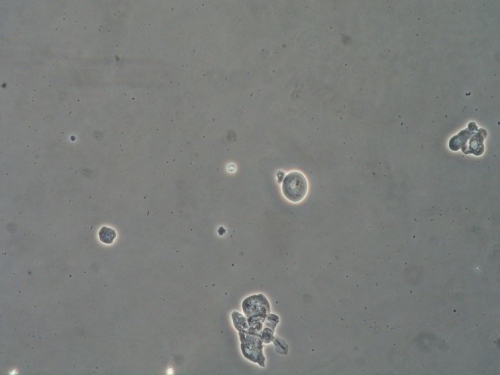
Microscopy:
Vaginal pH: 6.5
Wet prep: parabasal cells: 100%, clue cells absent, 0-1 WBCs per epithelial cell and absent lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM EXAM:
- Although she has a perineal fissure that is probably from the lichen sclerosus, and her lichen sclerosus is clearly not adequately treated, her pain is located mostly in the vestibule.
- Her age, postmenopausal status, and the pH and wet prep point to vulvovaginal atrophy as the primary cause of her discomfort.
- Urinary burning may be associated with atrophy, as well.
- Women do not need to be sexually active to benefit from the healing effects of vaginal estrogen in the postmenopausal period.
PRELIMINARY DIAGNOSIS:
- Biopsy-proven lichen sclerosus, not yet in good control
- Vaginal atrophy contributing to burning pain
- Possible irritation from base used for topical medications
Plan:
Testing sent or ordered: Yeast culture. Result: negative
Education: The patient was given handouts on general vulvar care, lichen sclerosus, and vaginal atrophy and her conditions were discussed. Advised to avoid irritants and irritants were specified.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days.
Treatment:
For the atrophy: Estrace cream, 1 gram inserted vaginally at bedtime for 14 days and then twice a week. Apply a small amount of the cream nightly to the vestibule, as well, on the same schedule.
For the lichen sclerosus: After 1 week of Estrace, start halobetasol 0.05%, a high potency topical steriod, applied in a thin film to all the whitened, fissured tissue nightly for 2 weeks and then every other day until your next visit.
To call the office if the burning gets worse.
Return visit findings:
One month later:
Soon after the first visit, she had called to report that halobetasol caused burning and she was switched to clobetasol 0.05% compounded with a petrolatum base that was comfortable for her. She was tolerating the Estrace cream, but thought that the discharge that dripped out the day after using it was causing some perianal irritation. Her pain level was down from a 9/10 to a 3/10.
She still had whitening on exam and some pain with q-tip touch, but she was more hopeful about recovery.
Assessment:
Improved pain with treatment of atrophy; ongoing inadequately treated lichen sclerosus
Plan:
Continue with compounded clobetasol three times a week; switch from vaginal Estrace cream to Vagifem 10 mcg inserted vaginally twice a week. Continue topical Estrace cream ¼ inch from the tube applied twice a week. Return visit in three months. Yeast culture sent and negative.
Two months later:
The patient reported ongoing burning sensations at a 2-3/10 level. She was happy with her results. She was using the compounded clobetasol Monday, Wednesday, and Friday and the Vagifem and topical Estrace Tuesday and Thursday. All the whitening had cleared up. She had increased erythema in the perineal area. pH and wet prep reflected adequate estrogen levels in the vagina.
Q-tip touch showed improvement in pain.
Assessment:
Improvement in burning pain and atrophy; lichen sclerosus in good control; ongoing burning possibly related to secondary vulvodynia
Plan:
Try nightly compounded clobetasol again for two weeks to see if burning will resolve. Then reduce the steroid ointment to three times a week again. Vulvodynia and possible treatment with a tricyclic antidepressant or anti-seizure medication discussed. Patient declined centrally acting oral medication. Yeast culture sent and negative. Follow up in four months.
Five months later:
Patient reports ongoing improvement. She is comfortable day to day, without burning or itching. She finds if she misses a Vagifem dose, she feels more uncomfortable.
Exam shows new whitened area on edge of the prepuce of clitoris. pH 4.7 and wet prep shows good estrogenization.
Assessment:
Atrophy and lichen sclerosus stable on regimen; small area of active LS
Plan:
Continue thrice weekly compounded clobetasol 0.05%, with special attention to prepuce; continue Vagifem, but increase dose to three times weekly; Continue topical Estrace cream twice a week. Yeast culture sent and negative. Follow up every six months.
Three years later:
The patient had been doing well on her own and had her own gynecologist check her LS and atrophy. However, she had had flaring symptoms of itching and irritation recently.
On exam, the labia majora were seen to be reddened uniformly, as if “sunburned.” The lichen sclerosus was in good control, with no further loss of tissue and no whitening. The pH and wet prep showed good estrogenization. No sign of yeast. Q-tip touch test showed mild irritative symptoms on the labia majora.
Assessment:
Atrophy and lichen sclerosus in good control; mild steroid rosacea or irritant skin reaction
Plan:
The patient was shown with a mirror where to apply her cream and ointment. She was advised not to apply the steroid to the outer labia majora. She was also advised to start “soak and seal” at least once a day, patting dry gently, then applying plain Vaseline to the skin of the outer vulva and vestibule. She was advised to cut back on the clobetasol, Vagifem, and Estrace to twice a week for all meds. Yeast culture was done and negative.
She returned two months later, completely comfortable, with no burning, no itching, no further anatomical or skin changes, and improved color and texture to the skin of the labia majora.
She has been asked to return every six months for routine surveillance.
TEACHING POINTS:
- Because of the 3-5% risk of women with lichen sclerosus developing squamous cell carcinoma, they need to be evaluated every six months on a routine basis, to check for ulceration or for thickened white plaques, as well as for control of the LS itself.
- We always try to use the least amount of medication necessary to control the condition.
- This patient had developed steroid rosacea from using the medication in the wrong place and using too much. It is important to show the patient with a mirror where to place the ointment, touch her skin in those areas for sense memory, and also give her a drawing showing correct placement. Show her, using plain lubricant, exactly how much to use.
- We initially tried a different brand of steroid, same strength. When she, again, had burning, we tried a compounded steroid in a neutral base (petrolatum) known not to cause skin reactions.
- This woman is not sexually active, but using a topical estrogen makes her more comfortable.