#2: Dyspareunia
Age, G/P, relationship status, occupation: 27 year old, G1 P1 by C/S, married MBA student, working part time in a financial office.
Menstrual status: Not getting periods because she is breastfeeding their first child, now 11 months old.
Contraceptive method: None now; she has used the OCP in the past to regulate her periods. She has been told that she has polycystic ovarian syndrome in the past.
Sexuality status: Male partner. Unable to have intercourse at all now.
Chief complaint: Painful intercourse; difficulty with penetration: very sore and sensitive
Symptoms (HPI: history of present illness): The patient reports discomfort with sex when she was younger which seemed to get better over time. Occasionally, in this relationship, she would have pain with insertion or discomfort afterward, which did not concern her much. She became pregnant and had a baby by Cesarean section 11 months ago. She is breastfeeding, working, going to school. Ever since she had the baby, she has not been able to have intercourse. She has tried abstaining from sex to let her body recover, different lubricants, only cotton underwear, and Free and Clear detergent. She never wears daily panty liners. She does feel that she has had a number of yeast infections and she recently used Monistat, leading to more symptoms of itching and irritation. She was seen by her doctor last month and Affirm testing did not show yeast, but did show Gardnerella. She was treated with Metrogel for that. She has not started using any contraception yet because of her pain. The patient says she has no lack of libido. She and her husband have a great relationship and are very happy together. She is quite upset about not being able to have sex with him. No discomfort with other activities of daily living.
Lifestyle issues: Honest or 365 unscented bath soap, and Country Safe or Honest detergent
History and review of systems:
- Vulvovaginal history: yeast and bacterial vaginosis. She reports no history of genital injury or trauma, no history of sexual abuse or assault
- GYN history: ASCUS on Pap in the past: benign. Ovarian cyst, resolved. Polycystic ovarian syndrome.
- Past and current medical conditions: Hypothyroidism, asthma as a child,
- Past surgical history: uncomplicated Cesarean section, appendectomy, tonsillectomy.
- Review of associated systems:
- Urinary: no problems
- GI: no problems
- Musculoskeletal: no problems
- Dermatological: no problems
- Mental health: concerned about vulvovaginal problem
- Review of other systems: Negative
- Social history: No smoking, drinking, use of recreational drugs. Walks daily.
Medications:
- Prenatal vitamins
- Iron supplementation
Allergies:
- No known allergies
KEY POINTS FROM HISTORY:
- Dyspareunia and concomitant breastfeeding are the red flags.
- She has a history of irregular periods in the past related to PCOS. This is probably not related to dyspareunia.
Non-genital exam:
BMI: 25.0 kg/(m^2). Vital signs within normal range
GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Exam: tolerated with discomfort
Groin: normal skin color and texture
Mons pubis: normal, non-tender.
Labia majora: normal skin color and texture and normal anatomy.
Perineum: normal skin color and texture and normal anatomy.
Anus: normal skin color and texture and normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: normal architecture bilaterally, normal skin color and texture
Prepuce: normal and mobile.
Clitoris: visible.
Interlabial folds: normal skin color and texture and normal anatomy
Vestibule: tender to q-tip touch test, uniformly erythematous, and unusually smooth texture
Urethral meatus: normal size, normal location, no masses.
Vagina: inflamed and tender to touch; Discharge: scant and white.
Pelvic Floor: hypertonicity is present and the patient has pain with exam
Cervix: deferred for pain
Uterus: deferred for pain
Adnexa: deferred for pain
Rectal: not indicated.

Microscopy:
Vaginal pH: 5.0
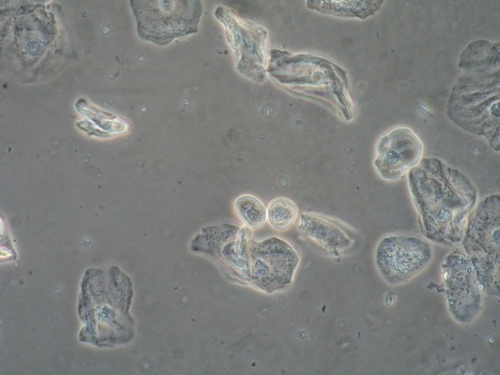
Wet prep: some normal epithelial cells, but 30% parabasal cells, one WBC per epithelial cell, no clue cells, no yeast seen, no trichomonas, absent lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM EXAM:
- The erythematous vestibule with its thinned epithelium and tenderness to touch, along with the inflammation in the vagina, plus the parabasal cells and absence of lactobacilli on wet prep clearly point to atrophy related to breastfeeding.
- Yeast must always be ruled out because it, too, can cause erythema and parabasal cells on wet prep. However, yeast is unusual in the setting of atrophy related to low estrogen states.
PRELIMINARY DIAGNOSIS:
- Lactational atrophy
Plan:
Testing sent or ordered: Yeast culture; Results: negative
Education: The patient was informed that atrophy, (as well as decreased libido in many women), is normal in the breastfeeding mother. It was up to her whether she wanted to wait until her body returned her to a more “estrogenized,” and therefore more comfortable state, or whether she wanted to use vaginal estrogen to hasten her ability to have intercourse. She was advised to start a birth control method prior to re-starting intercourse.
Restoration of the epithelial barrier: Application of a thin layer of Vaseline was suggested after every shower (or as often as desired) to moisturize the skin.
Treatment: topical estrogen cream (Estrace 0.01%), ¼ inch from the tube applied to the vestibule nightly for seven days then twice weekly, as well as 1/2 gram inserted into the vagina nightly for seven days, then twice a week until seen again was offered.
She was also offered Lidocaine 5% ointment to apply to the vestibule for about 10 minutes prior to wiping it off and applying a lubricant before trying intercourse.
Like many women, the patient preferred not to treat the atrophy. Once she understood that it was a natural accompaniment to lactation, and that there was nothing “wrong” with her, she preferred to try the Lidocaine alone.
Return visit findings:
She did not return for another visit. In reviewing the chart a couple of months later, it could be seen that she had called in to discuss weaning and contraception with her provider.
TEACHING POINTS:
- Lactation causes a drop in estrogen levels and an increase in progesterone and prolactin levels (as well as secretion of oxytocin with breastfeeding) that work together to promote breast milk supply, the let-down reflex, bonding with the baby, inhibition of ovulation, vaginal atrophy, and, often, temporary lack of libido.
- It is very helpful to educate the patient (and her partner) about these normal, temporary changes, especially in the woman who breastfeeds for a prolonged period of time. Many of these women, if not aware of these changes, blame themselves for lack of interest in sex and are confused by ongoing pain occurring long after childbirth healing is expected to have taken place.