#15: Itching and burning
Age, G/P, relationship status, occupation: 30 year old, G0, single, customer service agent
Menstrual status: Regular, monthly menses
Contraceptive method: Withdrawal or condoms
Sexuality status: Not in a relationship but has a “buddy,” a male sexual partner
Chief complaint: Vulvar itching and burning
Symptoms (HPI: history of present illness): Symptoms started about two years ago. She noticed some stinging one day when she was bathing and ran her hand over the left labium majus. She then started to get increasingly frequent episodes of itching and irritation that caused redness, stinging, burning, and soreness, sometimes accompanied by tiny white bumps in the irritated areas. She would be awakened at night by the itching. The left side of the vulva seems to be the worst. Intercourse is possible but she often had pain with intromission and persistent burning afterward that may last for a whole week. She has been treated four times over the last two years for BV and given an antifungal medication at the same time. She was treated recently with Clotrimazole with Betamethasone 1%/0.05% for two weeks and had some relief, but then the symptoms came back. She used to use daily panty liners but stopped a couple of months ago on advice of her doctor. She implemented other lifestyle changes, as well, such as switching from Ivory to Dove for Sensitive Skin soap and using unscented, non-coated menstrual pads. Genital cultures have been negative. She was treated for Chlamydia a year ago. She uses condoms for contraception, but inconsistently. Because of the persistence of her symptoms, she was given a prescription for Gabapentin (for hyperpathic itching), but has not started it because she knew she was coming in to this office and wanted to see what we would say. Her symptoms are not really present today, but she shows me a photo she took with her phone when they were acutely present and the vulva was quite reddened and swollen.
Pain symptoms on a scale from 0-10 at its worst: 5 out of 10
Symptoms of itching on a scale from 0-10 at its worst: 5 out of 10
Lifestyle issues: she uses Dial soap and Tide detergent; no daily panty liners.
History and review of systems:
- Vulvovaginal history: Yeast and bacterial vaginosis in the past; chlamydia treated a year ago, without recurrence. No history of injury, trauma, or abuse.
- GYN history: Pap smears have been abnormal: she had LGSIL five years ago with colposcopy showing CIN 1. She has had two Paps with ASCUS with negative high risk HPV; the rest of her Paps, including recently, have been normal.
- Past and current medical conditions: Vitamin D deficiency, exercise-induced asthma, headaches, (sometimes associated with right sided facial pain), depression and anxiety; she sees a therapist.
- Past surgical history: Negative
- Review of associated systems:
- Urinary: No symptoms
- GI: No symptoms
- Musculoskeletal: No symptoms
- Dermatological: No symptoms
- Mental health: Anxiety and depression, concern about vulvar condition
- Review of other systems: Negative
- Significant family history: her maternal grandmother has lichen sclerosus
- Social history: Lives alone; non-smoker, rare alcohol, no recreational drugs, does leg and arm stretches for exercise.
Medications:
- Multi-vitamins
Allergies:
- No known allergies
KEY POINTS FROM HISTORY:
- Treatment for bacterial vaginosis without coverage for yeast that occurs from antibiotic use might be a red flag for yeast, but she was consistently given an anti-fungal when treated for BV.
- The chronicity of the itching, and the awakening from sleep because of it, points to a possible dermatosis such as lichen sclerosus (especially since there is a family history) or the condition lichen simplex chronicus.
BMI: 18.29
Non-genital exam:
Back: Normal alignment of the spine, no lesions; Skin and nails: clear without lesions; Mouth: no oral or gingival lesions; Neck and thyroid: supple, no masses; Abdomen: soft, non-tender, no organomegaly; no tenderness to palpation over the bladder; Groin: There are no inguinal lesions or nodes
Genital exam and symptom mapping: (the patient has itching and burning throughout the vulva, but especially in the left interlabial sulcus)
Mons pubis: normal, non-tender.
Labia majora: normal anatomy and slightly lichenified.
Perineum: normal anatomy and slightly lichenified; itchy to touch.
Anus: normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: normal architecture bilaterally, mildly erythematous; there are sebaceous cysts under the skin, varying in size from a pin-point size to approximately 3 mm on both the interior and exterior aspects.
Prepuce: normal and mobile.
Clitoris: visible.
Interlabial folds: slightly erythematous; there is a darkened strip of skin on the left side where the skin is especially itchy
Vestibule: non-tender to q-tip test, slightly erythematous; itching and burning present
Urethra: normal size, normal location, no masses, no tenderness.
Vagina: well estrogenized, not inflamed and non-tender; Discharge: white. Non-odorous
Pelvic Floor: there is no hypertonicity.
Cervix: no lesions, no cervical motion tenderness.
Uterus: midline, mobile, smooth, non-tender, not enlarged.
Adnexa: not enlarged, no masses felt, non-tender.
Rectal: not indicated.


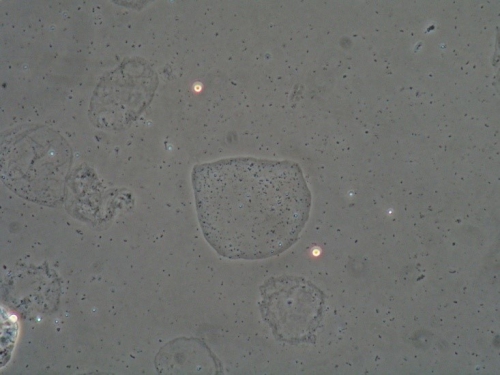
Microscopy:
Vaginal pH: 4.7
Wet prep: normal epithelial cells, parabasal cells: 0%, clue cells absent, no yeast forms seen, 0 WBCs per epithelial cell, few lactobacilli present, overgrowth of other bacteria present (mobiluncus) and trichomonas absent
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM EXAM:
- There was no sign of yeast under the microscope.
- Amsel’s criteria for BV were not met (no whiff, normal appearing discharge) but there were signs of mild BV (overgrowth of mobiluncus, few lactobacilli, absence of WBC’s)
- In dark skinned people, erythema and lichenification can look like darkened, rather than reddened skin.
- Anatomical exam was normal; the lichenification and erythema and chronic nature of the itching pointed to lichen simplex chronicus.
PRELIMINARY DIAGNOSIS:
- Lichen simplex chronicus
- Mild bacterial vaginosis
Plan:
Testing sent or ordered: Yeast culture; Results: negative; Herpes titer; Results: negative.
Education: Patient given handouts on general vulvar care, lichen simplex and on BV: Taught that LSC is an eczema-like skin condition caused by the itching from a yeast infection or from some other irritant and then made worse by scratching so that it becomes its own condition. Scratching must be stopped to heal.
Taught: Eliminate irritants such as tight clothing, daily panty liners, underwear to bed, thongs, feminine hygiene products, strong detergents, etc. Be gentle to your skin.
Taught: Bacterial vaginosis is likely to be recurrent in some women when condoms are not used consistently.
Discussed need for reliable contraception unless she wants a pregnancy.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days.
Treatment of lichen simplex chronicus: Betamethasone Valerate 0.1% ointment (about the size of 1/2 a pea) spread all over the itchy parts of the skin in a very thin film, twice a day for 14 days, then once a day for 14 days, then twice weekly till next visit.
In between using the Betamethasone, to use topical Vaseline: plain petroleum jelly.
To help with itching at night, Atarax, 10 mg at bedtime, orally, until itching is better. Benadryl as an alternative.
To help with itching at any time: topical Lidocaine 5%.
To prevent yeast: weekly Diflucan 150 mg orally.
Treatment of mild bacterial vaginosis: no treatment at this time; advised to use condoms.
One and a half months later:
The patient was not improved. She complained of ongoing itching and burning.Yeast culture and herpes titer from the first visit were negative. The patient’s treatments since the last visit included topical Betamethasone in a tapering dose, plus warm soaks, Vaseline, Atarax at night to help with itching, and weekly Diflucan for 4 weeks. The pt was very depressed about this. She and her partner had not been sexually active. She complained of extreme soreness and heat on the left side in the interlabial space adjacent to and just below the clitoris, spreading to the left labium minus. She also continued to have itching. She felt that the Betamethasone helped temporarily when she used it but then the effect would wear off.
Exam: Labia minora: normal architecture bilaterally, the right side looked normal in color, texture, and integrity and felt normal to the patient. Pain experienced in the left outer aspect of the labium minus into the interlabial sulcus up adjacent to the clitoris. The skin in this area was darkened at the first visit, but was less dark at this visit. There was less erythema in comparison with her photo.
Prepuce: normal and mobile. Clitoris: visible. Interlabial folds: normal skin color and texture on right side, erythematous, darkened (though improved) and very tender to touch. Vestibule: The vestibule was non-tender to q-tip test, normal skin color and texture; Vagina: not inflamed. Menses present.
Vaginal pH: 4.0
Wet prep: normal; one WBC per epithelial cell, no clue cells, no parabasal cells, no pathogens, normal lactobacilli; KOH: negative whiff and negative for pseudohyphae or spores
Assessment:
Lichen simplex chronicus, still not in control
Secondary vulvodynia
Mild BV on last exam, resolved
Plan:
Advised to watch for triggers and avoid them: tight clothing, chafing, sitting too long, scratching at night, etc.
Continue the warm soaks and topical Vaseline at the other end of the day from the steroid ointment. Betamethasone stopped. Advised to use the more potent Clobetasol 0.05% ointment in a thin film, twice a day, preferably after the warm soak and patting dry, for 30 days, then twice a week. If helpful, but only when used more often, to use it every other day until seen again.
Discussed secondary neuropathic pain. She was going to go back on an antidepressant for her mood anyway. Decision made to hold off on other treatment to see if antidepressant useful. Advised she would not be able to take oral Diflucan while on antidepressant. Clotrimazole advised. To call for increased itching, possible yeast infection.
Three and a half months later:
She was improved. She never started the anti-depressant. Yeast culture from last visit was negative. She had used Clobetasol twice a day x 30 days, then once a day every other day. She still felt that the area just outside the clitoris on the left was irritated and sore, with a burning sensation. She was using topical Lidocaine, which was helpful. She had tried to implement lifestyle changes, as well.
On exam: Prepuce: normal and mobile. Clitoris: visible. Interlabial folds: there was a subtly whitened patch in the left interlabial sulcus running from 3:00 up to 12:00 around the clitoral area. This is where she felt persistent itching. Vestibule non-tender to q-tip test, normal skin color and texture. Vagina: well estrogenized, not inflamed and non-tender; Discharge: normal and white. Pelvic Floor: there was no hypertonicity..
Vaginal pH: 4.0
Wet prep: normal; one WBC per epithelial cell, no clue cells, no parabasal cells, no pathogens, normal lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
Assessment:
Lichen simplex chronicus, improved
Possible early lichen sclerosus could not be ruled out
Reduction in neuropathic pain
Plan:
To continue the Clobetasol once a day now for another 30 days, then take it down to once a day M, W, F. Then, if really better, down to twice a week.
Six months later:
She was improved, but not perfect. Some days were better than others. She had not tracked her symptoms to see what made things better or worse. Yeast culture from last visit was negative. Treatments since the last visit included topical Clobetasol every other day, Atarax at night some nights (since the itching seemed worse at that point), warm soaks and topical Vaseline. Intercourse was not a problem for her. When she thought about it, she thought that sitting a lot (8 hrs a day at work) and having her pubic hair compressed against the area made it worse.
Exam: Interlabial folds: there was a strip of whitened tissue (subtle) on the left side that looked a bit longer than it did at the last visit. Vestibule non-tender to q-tip test, normal skin color and texture and normal anatomy.
Vaginal pH: 4.0 Wet prep: normal; one WBC per epithelial cell, no clue cells, no parabasal cells, no pathogens, normal lactobacilli; KOH: negative whiff and negative for pseudohyphae or spores
Assessment:
Lichen simplex chronicus, still not resolved, or early lichen sclerosus
Plan:
1) Switch to Halobetasol 0.05% and increase the frequency again to twice daily for the next two weeks. Then reduce it again to three times a week.
2) Lidocaine up to 5-6 times a day as needed.
3) Atarax renewed to help with itching/scratching at night, to take only if needed.
Seven months later:
She called to report that her symptoms were back and she was discouraged. She was instructed to stop the steroid ointment for two weeks and then come in for biopsy.
Two weeks later:
Patient presented for vulvar biopsy due to persistent swelling, itching and burning in the vulvar skin despite the use of steroid ointments. She had had a bad flare since her last visit. She did use more frequent halobetasol on it with temporary relief. But that flare was what convinced her to come in for a biopsy. She had been going through this for a long time without resolution of symptoms. When she flares, she gets swelling, redness, irritation, itching. She brought in a cell phone photo taken during her last flare.
Exam: The area where she was most symptomatic was to the left of the clitoris and a little bit below that level in the space between the prepuce and the labium minus. Skin color and texture slightly reddened in that area.
Biopsy done from the left interlabial sulcus at the site of most dominant symptoms with 3.5 mm Keyes punch. The patient was instructed in follow up care of the biopsy site and what to expect in terms of pain.
Biopsy result: lichen simplex chronicus
Plan:
The patient was called with her lab results: yeast culture was negative. Biopsy result confirmed lichen simplex chronicus. It was explained to her that if she could not stop scratching, she would not improve. Advised to cut her finger nails. Biopsy was healing well. Was painful for three days. Advised to continue warm soaks and topical Vaseline and not to put any steroid on the area until it is healed. Then go back to the halobetasol regimen we had last tried. To take Atarax at night and use topical Lidocaine prn. She was relieved to know she did not have something worse. Plan made to follow up by phone. Consider Gabapentin to help with neuropathic itching, especially since she had not started anti-depressant.
Consider getting the North American Series patch testing to see if she is having reactions to an allergen.
TEACHING POINTS:
- Retrospectively, it might have been helpful to the patient to have done the biopsy earlier. Doing a biopsy adds another 15 minutes to the visit for the time it takes the EMLA to numb the skin adequately before using injectable xylocaine, another five minutes for the procedure, and then another five to ten minutes to stop the bleeding from the procedure. It is not uncommon for vulvar specialists to make an educated guess at the diagnosis, treat, and then wait to biopsy if the treatment fails.
- Steroid ointment must be stopped for two weeks prior to biopsy for accurate results, except for the case of concern about possible malignancy.
- In this patient’s case, her lack of resolution of symptoms related to continued behaviors such as exposure to an unrecognized irritant or scratching (usually at night), or to the neuropathic part of her condition.
- If she does not get improved resolution in the next round, she will be offered treatment with oral Gabapentin starting at 100 mg orally, increasing by 100 mg a week up to 1,000 mg, with reassessment.
- Will also offer North American Series patch testing. See PDF for more information on this test.