#7: Unprovoked (spontaneous) pain
Age, G/P, relationship status, occupation: 42 year old, G0, married, bookseller
Menstrual status: regular menses
Contraceptive method: condoms
Sexuality status: 22 year marriage, supportive male partner, no previous history of dyspareunia. She has pain on penetration and post-coital pain, as well, for over a year.
Chief complaint: over a year of constant burning discomfort.
Symptoms (HPI): Patient has felt as if there were a “rug burn” over the vulvar skin and has the constant sensation that the skin would split open. She saw her gynecologist. A condyloma was removed without any change in symptoms and she had negative herpes titers. Her discomfort is always present except with her menstrual period. She awakens without pain but as the day progresses, the burning develops and progresses; she rates it as 7-8/10. Tight clothes bother and she can no longer use a tampon. She tried lidocaine 5% ointment without any change in her burning.
Lifestyle issues: had to stop working out on a stationary bicycle. No significant environmental irritants.
History:
- Vulvovaginal history: occasional yeast infection, vulvar condyloma, treated; negative HSV titers.
- GYN history: endometriosis by laparoscopy 14 years ago. On OCP for ten years; currently she has no pelvic pain or dysmenorrhea.
- Past and current medical conditions: excellent health
- Past surgical history: laparoscopy
- Associated review of systems:
- Urinary: negative
- GI: negative
- Musculoskeletal: back “muscle strain” after lifting box of books responded to physical therapy. Chronic lower back pain, well managed by daily stretching exercises. She has not had any imaging of her spine.
- Dermatological: negative
- Review of other systems: negative
- Social history: does not smoke or drink; walks one half hour daily
Medications: none
Allergies: no known allergies
KEY POINTS FROM THE HISTORY:
- Although she has a history of endometriosis, she does not complain of dysmenorrhea and pelvic pain. In fact, her vulvar pain improves during her menstrual period.
- Quantification of pain as 7-8/10 suggests severe pain.
- Consider back injury as a possible source of vulvar pain
Non-genital exam:
BMI: 25.0 kg/(m^2). Vital signs within normal range
GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Exam: well tolerated
Groin: normal skin color and texture
Mons pubis: normal, non-tender.
Labia majora: normal skin color and texture and normal anatomy. Patient points to location of unprovoked allodynia (pain) from the midline medially, down to the bases bilaterally.
Perineum: normal skin color and texture and normal anatomy.
Anus: normal skin color and texture and normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: normal architecture bilaterally, normal skin color and texture
Prepuce: normal and mobile.
Clitoris: visible.
Interlabial folds: normal skin color and texture and normal anatomy, but allodynia present bilaterally
Vestibule: non-tender to q-tip touch test, normal color and texture. No lesions.
Urethral meatus: normal size, normal location, no masses.
Vagina: not inflamed, non-tender; Discharge: scant and white.
Pelvic Floor: no hypertonicity
Cervix: no lesions, no cervical motion tenderness.
Uterus: midline, mobile, smooth, non-tender, not enlarged.
Adnexa: not enlarged, no masses felt, non-tender.
Rectal: not indicated.

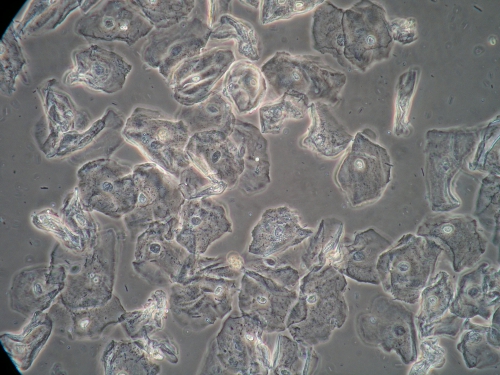
Microscopy:
Vaginal pH: 4.0
Wet prep: normal; one WBC per epithelial cell, no clue cells, no parabasal cells, no pathogens, normal lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM EXAM:
- Completely normal findings, (often with the exception of slight erythema) indicate vulvodynia.
- Candidiasis always needs to be ruled out.
- Post-herpetic neuralgia should be considered. In this case, we already had negative titers.
- The pain is “unprovoked (spontaneous) and generalized.” She has secondary dyspareunia.
PRELIMINARY DIAGNOSIS:
- Vulvar burning of unknown origin
- Probably unprovoked vulvodynia
Plan:
Testing sent or ordered: yeast culture: Results: negative
MRI of the lumbar and sacral nerve roots (see results below)
Education: about vulvodynia
Comfort techniques: loose clothing, avoidance of irritants, further work with lidocaine 5-6 times daily, soak and seal with topical Vaseline, cool packs
Treatment: Amitriptyline 10 mg at bedtime. Increase by 10 mg weekly to 50 mg weekly.
Topical Lidocaine 5% ointment applied up to five times a day as needed.
Return visit findings:
Three months later:
Yeast culture was negative and MRI showed mild degenerative disc disease without herniation or nerve root compression. Amitriptyline 50 mg was tolerated well except for constipation that responded to a fiber supplement and stool softener. Lidocaine was helpful for bad days. Her burning was reduced to 6/10. Her examination was unchanged.
Assessment: unprovoked vulvodynia with some improvement.
Plan: Repeat yeast culture. Increase the amitriptyline by 10 mg weekly to 100 mg at bedtime. Continue the lidocaine.
Six months later:
Repeat yeast culture was negative. Amitriptyline 100 mg was well tolerated. Lidocaine needed less frequently. Pain 5/10. Examination was unchanged.
Assessment: unprovoked vulvodynia with some further improvement but still flaring to 7/10 1-2 days weekly.
Plan: Repeat yeast culture. Add gabapentin 100 mg at bedtime and increase by 100 mg every 2-7 days depending on presence of sedation to 800 mg at bedtime.
One year after first visit:
Repeat yeast culture was negative. Medications were well tolerated and reasonable control 2/10 was gained with 600 mg gabapentin with the 100 mg amitriptyline. She was able to resume intercourse as the pain diminished.
She has been followed yearly for ten years with occasional pain flares controlled by transient increases of gabapentin by 100-300 mg, then returned to 600 mg daily after resolution of flare. Attempt to taper off medications brought pain flare.
TEACHING POINTS:
- The diagnosis of vulvodynia is made only when all other possible causes of vulvar pain have been eliminated.
- Obtaining numerical quantification of the pain is helpful in judging progress with management plan.
- Ongoing surveillance for Candida is important since it can cause bad flares of pain.
- Pelvic floor hypertonicity was not a feature for this patient.
- Neither the tricyclic antidepressants nor the anti seizure drugs like Gabapentin help with the pain of vulvodynia for everyone, but they do for some.