#19: Burning, dyspareunia
Age, G/P, relationship status, occupation: 66 year old G2 P2 (both vaginal births), married, cardiac sonographer.
Menstrual status: Postmenopausal since the age of 57
Contraceptive method: N/A
Sexuality status: Male partner, married 16 years. Not sexually active for the last six months. Never had discomfort with sex in the past.
Chief complaint: Burning in the vaginal area, extending out into the vulva
Symptoms (HPI: history of present illness): The patient says, “My symptoms started six months ago, after taking Amoxicillin (which I have never had a problem with in the past) for a cat scratch. We have five cats and I play with them, so I get a lot of scratches. I became very uncomfortable all of the time. I went to see my doctors and nurse practitioner and I tested negative for UTI, trichomonas, yeast, and bacterial vaginosis. A diagnosis of atrophy was made and I was asked to use Estrace cream once or twice a week applied to the vaginal opening in addition to the Vivelle 0.0375 mg/24 hr patch I have been using for at least three years. (She also uses Prometrium 100 mg, 1 po days 1-12 every three months and has withdrawal bleeds. Ultrasound has shown the endometrial stripe to be 3.6mm). One month ago, I started to use Lotrisone on my skin. My symptoms did not go away. I was asked to increase the topical Estrace cream to 3 times a week. Then, I was given Diprolene. The pain started to move up the sides of the vulva and I had some itching, too. Most recently, I was given Clobetasol, then Mometesone to use. The symptoms are worst in the morning when I wake up.” She also complains of dysuria. No frequency or urgency. (At the time of the visit, the patient was being treated with antibiotics for a laceration on her ankle.)
She has not had intercourse for six months. This is distressing to her although her partner is very understanding. Sex was never uncomfortable in the past.
Pain symptoms on a scale from 0-10 at its worst: 5 out of 10
Symptoms of itching on a scale from 0-10 at its worst: 1 out of 10
Lifestyle issues: Wears panty liners frequently to protect her underwear. Otherwise, no possible irritants. No underwear to bed.
History and review of systems:
- Vulvovaginal history: HPV on Pap smears. Has never even had a yeast infection. She reports no history of genital injury or trauma. She reports no history of sexual abuse or assault.
- GYN history: Being watched for LGSIL on Pap smear with positive HPV. Has had colposcopy. Otherwise, negative GYN history.
- Past and current medical conditions: abcess and cellulitis in hand and now on ankle,
- Past surgical history: Bunionectomy, septopasty
- Review of associated systems:
- Urinary: History of frequent urination and, recently, burning with urination
- GI: History of constipation and hemorrhoids; (not often; takes Metamucil)
- Musculoskeletal: Denies back injury, chronic back pain, arthritis, sciatica, herniated disc, back surgery, fibromyalgia.
- Dermatological: Eczema in her ears; no other issues.
- Review of other systems: Constitutional: no symptoms, EENT: no symptoms, Cardiovascular: no symptoms, Breasts: no symptoms, Respiratory: no symptoms, Endocrine: no symptoms, Neurologic: no symptoms, Psychiatric: no symptoms
- Social history: Alcohol: 6 drinks per week (wine with dinner); Cigarettes: non-smoker; Drugs: never; Exercise: treadmill
Medications:
- Estradiol (Vivelle-dot) 0.0375 mg/24 hr transdermal patch semiweekly
- Prometrium 100 mg, 1 orally days 1-12 every three months
- Ibuprofen 800 mg orally three times a day prn for pain
- Fluticasone 50 mcg/actuation Nasal Spray suspension: 2 sprays in each nostril once a day.
- Proctofoam HC (1-1%) rectal foam: Apply every 2-4 hrs as needed for hemorrhoids.
- Augmentin, 875-125 mg; 1 orally twice daily for cellulitis in laceration on her foot.
- Metrogel 1% topical gel: apply once a day to face.
- Momentasone 0.1% topical cream: apply topically once a day to the vulvar skin.
Allergies:
- Latex
KEY POINTS FROM HISTORY:
- The obvious initial considerations are possible atrophy despite systemic estrogen, which often does not reach the vestibule, yeast that has occurred due to antibiotic treatment of the ankle and face, or steroid overuse.
Non-genital exam:
BP 110/74 | Ht 5′ 4″ (1.626 m) | Wt 133 lb (60.328 kg) | BMI 22.83 kg/m2; GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Exam is tolerated with discomfort.
Mons pubis: normal, non-tender. Anterior commissure normal.
Labia majora: normal skin texture and normal anatomy. There is reddening of the skin superficially seeping up from the base of the vaginal opening up the labia minora and majora with irregular edges.
Perineum: normal skin color and texture.
Anus: normal skin color and texture and normal anatomy. Flaccid hemorrhoid.
Bulbocavernosus reflex and anal wink present.
Labia minora: normal architecture bilaterally, slightly erythematous; ;non-tender.
Prepuce: normal and mobile.
Clitoris: visible.
Interlabial folds: erythematous
Vestibule: The vestibule is tender to q-tip test at 6:00 and throughout the vestibular clock, erythematous posteriorly but pallid anteriorly
Urethra: normal size, normal location, no masses, no tenderness.
Vagina: poorly estrogenized and tender; Discharge: scant.
Pelvic Floor: hypertonicity is present.
Cervix: multiparous appearance and no cervical motion tenderness.
Uterus: midline, mobile, smooth, non-tender, not enlarged; retroverted.
Adnexa: not palpable.
Rectal: not indicated.
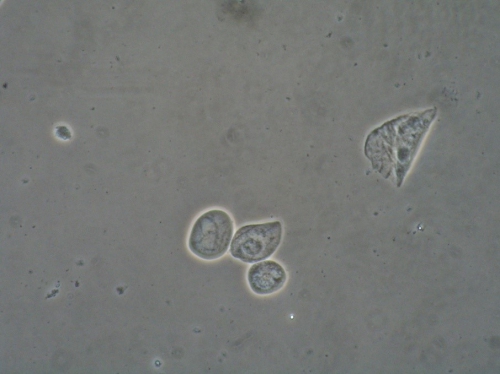
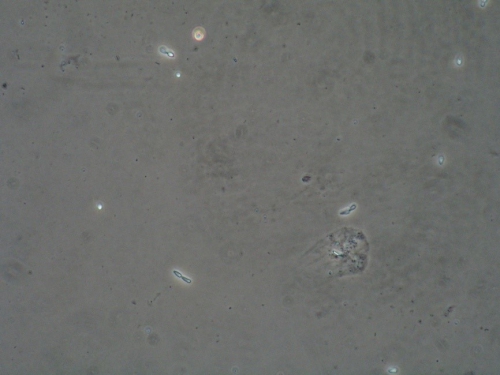
Microscopy:
Vaginal pH: 6.5
Wet prep: parabasal cells: 98%, clue cells absent, no yeast forms seen, 1 WBCs per epithelial cell, absent lactobacilli and trichomonas absent
KOH: negative whiff and negative for pseudohyphae or spores
Clinical photo documentation done with consent.

KEY POINTS FROM EXAM:
- The assessment of vaginal and vestibular atrophy was based on the wet prep and the physical exam.
- Because the erythema “spilled over” outside the edges of the epithelium usually affected by atrophy, and the pt had been using a lot of steroid ointment, steroid rosacea was suspected.
PRELIMINARY DIAGNOSIS:
- Vaginal and vestibular atrophy, not being reached by the HRT she is using.
- Mild steroid rosacea from using too much steroid ointment
Plan:
Testing sent or ordered: Yeast culture: Results: negative Urine culture: Results: negative.
Education: Patient given handouts on general vulvar care, vaginal atrophy, and the use of steroids in vulvar care. Instructed to avoid irritants.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days, then once a day as frequently as possible.
Treatment: Stop the steroid treatments. Start using Vagifem 10 mcg tablets inserted vaginally nightly for seven nights, then three times a week. Also, apply Estrace cream, ¼ inch from the tube, topically to the vestibule nightly for seven nights, then three times a week.
Return visit findings:
Eight weeks later:
The patient had been compliant with the treatments. She was feeling no better. Unable to have sex.
Exam: (abnormal findings only)
Labia majora: there was still a reddened plaque on the right labium majus, extending up into the mons. The skin on the left had a little erythema but mostly looked normal.
Vestibule: tender to q-tip test at 6:00, erythematous with a small white lacy pattern there. Slightly swollen on the right and adjacent to that, there is a tiny white patch that looked a bit like a collapsed blister or a plaque.
Vagina: well estrogenized, slightly inflamed and tender; Discharge: scant.
Pelvic Floor: hypertonicity is present.
Microscopy
Vaginal pH: 5.3
Wet prep: normal epithelial cells, parabasal cells: 20%, clue cells absent, no yeast forms seen, 1-2 WBCs per epithelial cell, many lactobacilli present, especially elongated LB, common with estrogen replacement, and trichomonas absent
KOH: negative whiff and negative for pseudohyphae or spores
Biopsy done:
1% xylocaine used for local anesthesia after betadine prep.
Vulvar biopsy obtained with 3.5 mm Keyes punch from the fourchette at 6-7:00.
Hemostasis achieved by pressure and AgNO3.

KEY POINTS FROM EXAM:
- The pH and wet prep had improved, but not as much as would be expected from the use of topical estrogen as an adjunct to systemic estrogen (via the patch). There were good lactobacilli and reduced numbers of parabasal cells, but the pH continued to be elevated with ongoing parabasal cells. Hence the diagnosis of DIV.
- Yeast was not seen under the microscope, but the presence of yeast may also cause increased numbers of parabasal cells.
- The tiny white patch did not look “regular or familiar.” That is why decision for biopsy was made.
- Retrospectively, it would have been good to have taken another photo prior to doing the biopsy.
Assessment:
Vaginal atrophy in good control.
Desquamative inflammatory vaginitis
Vulvar lesion: possible lichen planus; rule out VIN
Plan:
Yeast culture sent. Biopsy of tiny white patch at 6-7:00 offered and accepted.
Education: Handouts given on biopsy after-care and on desquamative inflammatory vaginitis (DIV).
The plan was to have the patient use vaginal Anusol 25 mg hydrocortisone suppositories nightly for 14 days, the every other day until seen again, in conjunction with the Vagifem twice weekly and Estrace twice weekly once the skin had healed from the biopsy.
Yeast culture result: Culture positive for C. parapsilosis. The patient was called and told NOT to use the vaginal Anusol, but to treat the yeast with Boric Acid capsules 600 mg at HS nightly for 14 days and to stop using the vaginal estrogen at the time of treatment for yeast.
Biopsy result: VIN II found at time of biopsy. Pt referred to a GYN oncology specialist.
Return visit findings:
Three months later:
The pt had been seen by GYN ONC three months previously, both for a consult with biopsies and then for treatment one month later. Prior to doing the treatment (skinning vulvectomy and laser), her doctor had repeated a number of biopsies, as well as a Pap smear. One biopsy at 7:00 in the vestibule showed VIN III. Another, in the mons pubis on the right side, showed lichen simplex chronicus. Prior to having the surgery, she also had a negative yeast culture. Her recovery was complicated by a strep throat a few days after discharge from the hospital. She was treated with antibiotics and developed a culture-proven yeast infection (C. Albicans), for which she took Diflucan. Recovery was also accompanied by pain from the procedure. At her follow up visit with the Oncology NP, she complained of ongoing vestibular pain and was told she had pelvic floor hypertonicity. She went to the recommended pelvic floor physical therapist, who could not do an exam on her because of pain. She then called us in confusion and we asked her to come in.
Exam:
The exam is tolerated with discomfort.
Mons pubis: normal, non-tender. The biopsy site in the right side of the mons was healing well. A suture was protruding out on two sides of the lesion. This was pulled out, with the pt’s permission, with no bleeding, no pain. Anterior commissure: normal skin color and texture and normal anatomy
Groin: normal skin color and texture and normal anatomy
Labia majora: normal skin color and texture and normal anatomy.
Perineum: normal skin color and texture and normal anatomy.
Anus: normal skin color and texture and normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: normal architecture bilaterally, normal skin color and texture except on the right side where the tissue is still healing from the procedure and is erythematous and tender to touch.
Prepuce: normal and mobile.
Clitoris: visible.
Interlabial folds: normal skin color and texture and normal anatomy
Vestibule tender to q-tip test at 5-7:00, erythematous; there is a bridge of tissue stretched abnormally at 6:00, not present at her first visit, and probably related to the treatment. PHOTO taken with the pt’s permission.
Hymenal ring: erythematous
Urinary meatus: normal size, normal location, no masses.
Vagina: not inflamed and non-tender; Discharge: scant.
Pelvic Floor: pt has pain with one finger palpation. Unable to evaluate the pelvic floor.
Microscopy performed using a phase contrast microscope shows:
Vaginal pH: 5.8
Wet prep: normal epithelial cells, parabasal cells: 5%, clue cells absent, no yeast forms seen, 2 WBCs per epithelial cell, many lactobacilli present and trichomonas absent
KOH: negative whiff and negative for pseudohyphae or spores

Assessment:
Pt healing from treatment of VIN III lesion in vestibule but having ongoing provoked vestibular pain
Inadequately treated atrophy or DIV on wet prep
Plan:
Resume use of Vagifem and Estrace cream twice weekly and return in 6 weeks.
Topical Vaseline morning and evening.
Yeast culture sent: Results: positive for C. Albicans again; patient called and told to hold off on estrogen again while taking Diflucan.
One month later, she became symptomatic with burning and sent in a yeast culture which was again positive for C. Parapsilosis. We asked her to, at that point, repeat the Boric Acid vaginal capsules, 600 mg nightly for 14 days again.
Return visit findings:
Two months later:
She has been feeling a lot better but has not resumed sexual activity though they both would like to. She is still afraid of having pain. Felt better after the treatment for C. Parapsilosis, but is beginning to feel symptomatic again with itching. Still on the Vivelle dot twice weekly with the prometrium every three months. No other treatment for atrophy.
Exam:
Normal with the exception of the interlabial sulci, which were itchy, and the vestibule:
Interlabial sulci: slightly erythematous.
Vestibule slightly tender to q-tip test at 5-7:00, erythematous with a bridge of tissue stretched abnormally at 6:00, not present at her first visit, and probably related to the treatment. White pattern present on the right side; ? scarring from surgical procedure.
PHOTO taken with the pt’s permission.
Pelvic Floor: no hypertonicity. Pt tolerated exam well.
Microscopy
Vaginal pH: 5.0
Wet prep: normal epithelial cells, parabasal cells: 50%, clue cells absent, no yeast forms seen, 2 WBCs per epithelial cell, many elongated lactobacilli present and trichomonas absent
KOH: negative whiff and positive for skinny budding, oval spores: probable Parapsilosis.

Assessment:
Patient doing well s/p surgical treatment for VIN III
Inadequately treated vaginal atrophy despite Vivelle patch
Possible DIV which can not be ruled in or out until she is treated for atrophy
Recurrent vaginal yeast, both Albicans and non-Albicans, this time looking like non-Albicans yeast
Lichen simplex chronicus
Plan:
Yeast culture sent. Results: confirmed C. Parapsilosis.
We tried treating the atrophy alone first, switching to Estrace cream 1 gram vaginally twice a week and topically twice a week, since the non-Albicans yeasts can turn up in poorly estrogenized post-menopausal women and don’t necessarily need treatment, but the patient called asking for treatment because she was having itching.
Treated with Diflucan 200 mg orally every other day x 3 then twice weekly, with ultimate eradication of the yeast.
Also given topical Betamethasone Valerate 0.1% for her biopsy-proven lichen simplex chronicus.
To continue warm soaks and topical Vaseline.
We discussed her going off of the Vivelle Dot and she planned to discuss this with her gynecologist.
Because of the whitened pattern on the right side of the vulva, I asked her to return to her oncologist for a check up.
Return visit findings:
Three months later:
The patient was feeling much better. She had been compliant with treatments. She had stopped the Vivelle Dot and was happy with the decision. Her Pap smear at the oncologist’s office was negative, as was acetic acid evaluation.
No further unprovoked itching or burning.
Still not sexually active, but hoping to try it.
Exam:
Physical exam was not that changed, but the pH was 4.5 and the wet prep was improved with only 5% parabasal cells and normal, elongated lactobacilli.
She had no pelvic floor hypertonicity and no pain on the exam.
She was advised to try lidocaine 5% ointment x 10-15 minutes prior to intercourse, wiping it off first and then applying a lubricant to help her gain confidence in her ability to have penetration without pain; she was advised to continue the Betamethasone Valerate 0.1% when needed and the Estrace cream 1 gram twice weekly and a small amount topically.
TEACHING POINTS:
- This case illustrates how important it is to listen to the patient and to continue to keep an open mind and a strict evaluation process going to properly diagnose.
- It also illustrates what happens when many clinicians get involved in the patient’s care. In some cases, we need each other, but in some cases, the patient needs to select her clinician and stay with one point of view.
- The evaluation process can take some time, and the clinician should keep an eye on the calendar and always ask him/herself if the decision making is cogent, if the treatment is working, and if there are any other possible diagnoses when issues go on for a long time. It is always possible to get a colleague’s opinion when unsure.
- Approximately 60 percent of women with vaginal intraepithelial neoplasia (VAIN) 3 or VIN have preexisting or synchronous cervical intraepithelial neoplasia (CIN), and close to 10 percent of women with CIN 3 have concomitant squamous intraepithelial neoplasm at other sites (e.g. 3 percent have VAIN 3 and 7 percent have VIN).1
- Vulvar intraepithelial neoplasia (VIN) presents with symptoms in many cases, but is often asymptomatic and is noted incidentally during pelvic examination.
- Vulvar pruritus is the most common complaint among symptomatic women. Other potential symptoms are vulvar pain or burning, or dysuria. Dysuria may occur if there is a periurethral VIN lesion or if urine comes into contact with a VIN lesion at another site. A systematic review of 97 studies including over 3300 women with VIN 3 reported that 64 percent presented with pruritus or pain.2
- Approximately 40 percent of women with VIN are asymptomatic and are diagnosed when a lesion is noted by the patient or detected during a routine gynecologic examination or at colposcopy for abnormal cervical cytology. A visible lesion or a palpable abnormality may be noted.3 There is no one characteristic with which to describe VIN, which is why it is called “the great masquerader.” It may be white, brown, pink, red, gray,or whitish in color and it may be macular, papular, or verrucous.
- A vulva with multiple areas of abnormalities warrants multiple biopsies.4
- Follow up of patients with VIN should take place every six months for five years because recurrence or new lesions may occur.