#14: Burning, irritation, dyspareunia
Age, G/P, relationship status, occupation: 68 year old, G1/P1 (SVD), married, retired teacher and school administrator
Menstrual status: postmenopausal
Contraceptive method: postmenopausal
Sexuality status: 34 year marriage, male partner, strong relationship, no prior dyspareunia. Currently, unable to be sexually active with vaginal intercourse.
Chief Complaint: rawness, irritation, dyspareunia
Symptoms (HPI): After a long history of frequency, urgency, and dysuria with “urinary tract infections,” sometimes without positive cultures, she was diagnosed with interstitial cystitis two years ago. At the same time, she was diagnosed clinically with lichen sclerosus and started on topical clobetasol.
Her bladder symptoms came into control with treatment. She felt that clobetasol helped her initially, but then she developed an external vulvar rash, that was diagnosed as yeast. Nystatin helped at times, but vulvar irritation never goes away. Rawness and discomfort persist and penetrative sex is impossible.
Lifestyle issues: irritants are not an issue.
History and review of systems:
- Vulvovaginal history: yeast infections, chlamydia treated in college. No history of HSV or HPV.
- GYN history: endometriosis and bleeding treated with total abdominal hysterectomy, unilateral oophorectomy, age 34. Pap smears normal.
- Past and current medical conditions: fibromyalgia, arthritis, hypertension,
- Past surgical history: hysterectomy and unilateral oophorectomy, carpal tunnel, thumb reconstruction, left knee meniscus
- Review of associated of systems:
- Urinary: clinically diagnosed interstitial cystitis, quiescent
- GI: GERD
- Musculoskeletal: Fibromyalgia
- Dermatological: History of dermatitis and pre-cancerous facial lesions
- Other review of systems: sinusitis, sleep apnea treated with CPAP
- Social history: No alcohol, no tobacco, no drugs, 3 hrs exercise/week
Medications: etodolac, bisoprolol, hydrochlorthiazide, omeprazole, cyclobenzaprine, zolpidem, hydroxyzine, phosphasal, nystatin cream, clobetasol ointment, tramadol, glucosamine, ergocalciferol
Allergies:
- Codeine
- Penicillin
- Sulfa
- Compazine
KEY POINTS FROM THE HISTORY
- Consider that the presence of painful bladder/interstitial cystitis often leads to pain in the vestibule since both bladder and vestibule arise from same source: the urogenital sinus.
- Consider that she is postmenopausal for years without estrogen; atrophy alone may cause dyspareunia, but it also can add to symptoms of a vulvar dermatosis such as lichen sclerosus.
Non-genital exam:
BMI: 25.0 kg/(m^2). Vital signs within normal range
GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Exam: well tolerated
Groin: normal skin color and texture except for scattered, pale, tan, macules on the left side, accompanied by “irritated” sensation.
Mons pubis: normal, non-tender.
Labia majora: normal skin color and texture and normal anatomy, but faint, white, crinkled, epithelium at labial bases at in anterior commissure and folds above clitoris.
Perineum: whitened, thickened. Non-tender.
Anus: normal skin color and texture and normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: absent bilaterally, skin erythematous
Prepuce: normal and mobile.
Clitoris: visible, exposed.
Interlabial folds: normal skin color and texture and normal anatomy
Vestibule: tender to q-tip touch test, uniformly erythematous, thin, dry, atrophic
Urethral meatus: normal size, normal location, no masses.
Vagina: pallid and tender to touch; Discharge: scant and yellow-white.
Pelvic Floor: no hypertonicity
Bimanual exam: cervix surgically absent; limited exam due to body habitus
Rectal: not indicated.

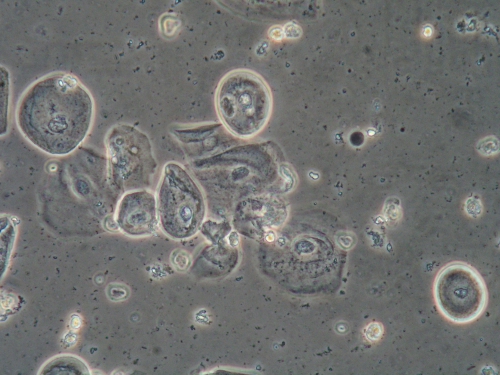
Microscopy:
Vaginal pH: 7.0
Wet prep and KOH: 50% normal epithelial cells, 50% parabasal cells, one to two white blood cells per epithelial cell, lactobacilli absent, no yeast forms, clue cells, or trichomonads.
KEY POINTS FROM THE EXAM
- Absence of labia minora are a sign of dermatosis: either lichen sclerosus or lichen planus.
- White, crinkled epithelium is also a sign of dermatosis.
- Erythema in vestibule can be from atrophy or lichen planus.
- Groin irritation seems to be a separate issue
PRELIMINARY DIAGNOSIS:
- Mild dermatitis in groin
- Marked vulvovaginal atrophy
- Clinically diagnosed lichen sclerosus
Treatment Plan:
Testing sent or ordered: yeast culture: Result: negative.
Education: about lichen sclerosus and vaginal atrophy and gentle vulvar care.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal in the hydration with Vaseline twice daily for 7 days. Advised to soak prior to application of the steroid ointment treatment for lichen sclerosus, as well.
Treatment of groin irritation: ciclopirox cream (emollient with antifungal activity) to the groin folds twice daily for 14 days, then MWF
Treatment of lichen sclerosus : clobetasol 0.05% ointment to the vulva and vestibule twice daily for 14 days, then MWF
Restoration of adequate local estrogen: estradiol cream (Estrace) 1/8 tsp to the vulva nightly, and 0.5 gram of estradiol cream inserted into the vagina nightly for seven days, then twice weekly for maintenance.
Return visit findings:
Two months later: More comfortable and less sensitive on the vulva, but there is still irritation in the vestibule and groin. The patient is compliant with estradiol around introitus and vaginally, clobetasol 0.05% MWF, and ciclopirox MWF in groin folds.
Exam: Left groin has narrow linear scaly plaque of 2 cm along panty line. Vestibule has a mild erosion with two 2mm muddy, white macules at 3 and 9 and a serpentine border. Vagina well estrogenized with normal pH and wet prep.
Assessment: groin dermatitis aggravated by underwear. At this visit, there is the classic appearance of lichen planus in the vestibule.
Plan: Switch to women’s boxer shorts without elastic. Apply iodoquinol (hydrocortisone with iodine for mild steroid and anti-bacterial effect) to the groin area twice daily for 14 d then MWF. Resume clobetasol 0.05% topically twice daily and add a dab of tacrolimus (Protopic) 0 .03% on top of clobetasol twice daily until next visit in two months.
Six months later: She did well with Protopic and clobetasol until her Protopic samples ran out. The insurance denied the prescription and the cost was $600 for 15 g. She continued the clobetasol twice daily MWF, and Estrace vaginally TTh and nightly to the vestibule. She is much better and has been able to have intercourse with reasonable comfort. Uses iodoquinol to the groin MWF. Likes women’s boxer shorts.
Exam: Both groins are free of lesions. Vestibule has erythema without erosion. No white reticulations. Vagina well estrogenized. Wet mount: normal epithelial cells, rare parabasal, 0-1 white cell per epithelial cell, normal lactobacilli, no pathogens.
Assessment: Groin dermatitis is in control. Lichen planus in the vestibule is better but still active.
Plan: Continue clobetasol twice a day MWF and file prior authorization for medical necessity for Protopic use. Continue estrogen cream one half gram vaginally Tues/Thurs and topically, nightly, in vestibule. Use iodoquinol in groin areas MWF.
12 months later: Doing well, comfortable. Compliant with clobetasol and tacrolimus (Protopic) MWF and estrogen cream one half gram vaginally twice weekly and nightly to vestibule. Uses iodoquinol twice weekly to groin areas.
Exam: both groins clear. Vestibule nontender, without erythema or lesions. Vagina well estrogenized.
Assessment: lichen sclerosus, lichen planus, and atrophy in control. Groin dermatitis clear.
Plan: Continue the clobetasol 0.05% with tacrolimlus 0.03% three times a week, iodoquinol twice weekly and estrogen cream 0.5 grams vaginally twice weekly and ¼ inch nightly to vestibule. Yeast culture was positive for Candida albicans and she was treated with fluconazole 150 mg day one and day four.
Two years later: continues comfortable, in control, sexually active with enjoyment. Asked to continue the same regimen for another year.
TEACHING POINTS:
- Education about the problem is essential to achieve successful treatment: most epithelial disorders are chronic; symptoms will return if treatment is discontinued; steroid use as directed is safe.
- Educate about gentle vulvar care, elimination of irritants, on-going management, calling before stopping a treatment that worsens or is not working.
- Candida albicans was not present initially but showed up after treatment with immune- suppressant topicals in combination with topical estrogen. Prophylactic suppression of Candida is often important when using steroids and estrogen. Routine check of culture for yeast at every visit is an important part of management. A single culture at the first visit is never adequate.
- The same vulva may show lichen sclerosus, lichen planus, and lichen simplex chronicus in different areas. In this case, irritant dermatitis from tight underwear was adding to symptoms.
- Restoration of the epithelial barrier is essential with any epithelial pathology.
- Adequate local estrogen is an important management tool.