#5: Dyspareunia
Age, G/P, relationship status, occupation: 27 year old, G0, married, health writer
Menstrual status: regular menses
Contraceptive method: OCP and condoms
Sexuality status: Unable to have vaginal intercourse because of pain. She indicated that she was able to be aroused and stimulated sexually but any contact in the vestibule produced extreme pain. She felt that her husband was supportive; he drove her to the visit, but did not come in for the consult. No history of physical, emotional, or sexual abuse.
Chief complaint: pain on penetration
Symptoms (HPI: history of present illness):
The patient had frequent itching and discharge in her teen years. She was treated on numerous occasions for Candida. At the age of fourteen, she attempted to use a tampon and was unable to insert it. She is still unable to use a tampon. She was not sexually active until she married and was on her honeymoon three years ago. Penetration was painful and the experience was disappointing.
She saw a gynecologist who gave her Vagifem and referred her for physical therapy to the pelvic floor. She worked with a physical therapist for six months without improvement and subsequently switched to another within the same practice. She thought she was starting to move forward with the new physical therapist. She denies any unprovoked pain but has a constant sense of vulvar irritation. She expresses frustration and concern that no one can help.
Lifestyle issues: irritants are not a problem
History and review of systems:
- GYN history: on OCP since age 18 to regulate menses; able to have Paps with pain with speculum. Paps normal. No history of STIs.
- Past and current medical conditions: Migraines since teens, thyroid nodules, exercise induced asthma, palpitations, fibromyalgia
- Past surgical history: odontectomy (tooth removal), repair of nasal septal perforation
- Review of associated systems:
- Urinary: denies
- GI: denies
- Musculoskeletal: history of herniated disc L4-5, with chronic back pain. Fibromyalgia diagnosed when she was age 17.
- Dermatological: denies
- Review of other systems: headaches, occasional palpitations
- Social history: never smoked, denies alcohol or recreational drug use; 3-4 hours of exercise a week
Medications:
- Multi-vitamins
- Duloxetine 60 mg orally daily for fibromyalgia and migraines
- Lo-Estrin OCP
Allergies:
- Sulfa
- Terconazole
KEY POINTS FROM THE HISTORY:
- Long-term history of itching and discharge may point to a dermatosis such as lichen sclerosus, eczematous dermatitis, or chronic inflammation in the vulva, any of which might have stimulated pain reactions.
- Early history of not being able to use a tampon or dyspareunia continuing past first week of penetrative sexual activity may indicate difficult-to-treat primary vulvodynia.
- In young women, lack of estrogen in the vagina is extremely rare if normal menstrual periods are present. This can be checked through the pH and the wet prep, which does not change due to the OCP.
- Chronic back pain can be related to pelvic floor dysfunction. Chronic pain conditions like fibromyalgia are a red flag for other chronic pain conditions.
Non-genital exam:
BMI: 32.5 kg/(m^2). Vital signs within normal range.
GENERAL: overweight female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Exam: tolerated with tension and anxiety
Groin: normal skin color and texture
Mons pubis: normal, non-tender.
Labia majora: normal skin color and texture and normal anatomy.
Perineum: normal skin color and texture and normal anatomy.
Anus: normal skin color and texture and normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: absent 2-5:00 and 7-10:00 with a thin ridge of tissue at 6:00; normal skin color and texture
Prepuce: normal and mobile.
Clitoris: visible.
Interlabial folds: erythematous
Vestibule: tender to q-tip test and erythematous from frenulum to fourchette
Urethral meatus: normal size, normal location, no masses.
Vagina: well estrogenized, not inflamed and non-tender; Discharge: normal and scant.
Pelvic Floor: hypertonicity and tenderness are present
Cervix: no lesions, no cervical motion tenderness.
Uterus: midline, mobile, smooth, non-tender, not enlarged.
Adnexa: not enlarged, no masses felt, non-tender.
Rectal: not indicated.

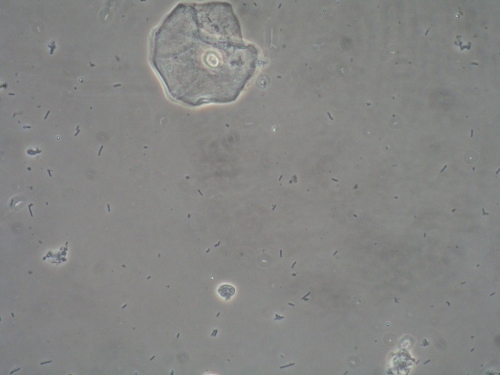
Microscopy:
Vaginal pH: 4.4
Wet prep: normal epithelial cells; one WBC per epithelial cell, no clue cells, no parabasal cells, no pathogens, normal lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
Vulvar biopsy: Keyes punch biopsy done at 4:00 in vestibule after application of EMLA and 1% xylocaine injected for pain relief.
PRELIMINARY DIAGNOSIS:
- Vulvitis, (biopsy pending for clarification)
- Localized, provoked vulvodynia
- Pelvic floor dysfunction as a cause, and as a result, of pain
Plan:
Testing sent or ordered: yeast culture and vulvar biopsy from vestibule at 4:00 in the vestibule. Results: negative yeast culture, non-specific inflammation on biopsy.
Education: Handouts given on vulvar pain/vulvodynia, the impact of pelvic floor hypertonicity on vulvar pain, vulvitis, and pelvic floor physical therapy and condition discussed.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days.
Treatment: “Soak and seal” with betamethasone valerate 0.1% ointment daily x 14 days, then betamethasone valerate 0.1% twice weekly. Call for test results in one week. Continue with physical therapy to the pelvic floor. Discussion of available supports, declined by patient
Return visit findings:
Three months later:
Yeast culture was negative and biopsy showed non-specific inflammation at the time of the first visit. She reported that betamethasone valerate was helpful. She had continued her physical therapy, and reported that biofeedback showed her pelvic floor muscle tension was normal. Medium dilator insertion was painful on insertion even with lidocaine. Her therapist was asking her to progress with dilators despite ongoing pain. Examination was unchanged. Valium 5 mg vaginal suppositories were ordered (to be inserted nightly) in view of significant pelvic floor muscle tightness and tenderness on exam in the office.
Five months later: Nothing had changed. She had ongoing tenderness in the vestibule and hypertonicity of the pelvic floor. Valium was of no help. Close questioning revealed that external electrodes were being used instead of vaginal electrodes for pelvic floor biofeedback, meaning that low muscle tension was reported, since only the bulbospongiosus and superficial transverse perineal muscle tensions were being measured. Ongoing pain with dilator use was also serving as a negative reinforcer. She was asked to continue the betamethasone valerate 0.1% twice weekly, to stop physical therapy with the current provider and to go back to a small dilator with lidocaine; not to use it if it caused pain. She was referred to a new physical therapist.
11 months later: Her physical therapy had been stalled by a concussion. Examination was unchanged. She was ready to move forward with treatment.
16 months later: EMG resting voltage was normal and she felt that she had made some progress. There was still pain on penetration. Vulvar erythema was lessened; hypertonicity was still present.
28 months later: She had continued to make progress, but was in treatment for thyroid cancer.
After 2.5 years: She was discharged from physical therapy, pain free. She had divorced her husband and had a new partner with whom she was having pain-free intercourse. Her examination was normal: no tenderness, no erythema. After 4 years, she is doing well. She has continued the steroid once weekly; without it, she has irritation. She is free of dyspareunia.
Teaching points:
- Vulvovaginal pain can be difficult to diagnose and to treat. The steps of the algorithm must be implemented at every visit to come to the correct diagnosis. If the exam is completely normal, but pain or dyspareunia persist, there are still tests that can be done, medications and approaches that can be tried.