#8: Dyspareunia
Age, G/P, relationship status, occupation: 22 year old, G0, single marketing specialist, living with her boyfriend of two years.
Menstrual status: regular menstrual periods
Contraceptive method: OCP: Tri-Sprintec
Sexuality status: male partner; sexually active as she can tolerate it.
Chief complaint: pain after intercourse
Symptoms (HPI: history of present illness):
The patient says that approximately three months ago, she woke up one morning, out of the blue, with severe burning and throbbing after intercourse. She thought she had a bad yeast infection and self-treated with Monistat without benefit. She went to her PCP who prescribed Diflucan but this did not help. She took more Diflucan but it still did not help. She was then treated for bacterial vaginosis with Clindamycin, again with no benefit. She was referred to another doctor who diagnosed her with non-Albicans yeast and treated her with Terazol. Her tests for BV, trichomonas, and yeast came back negative, as did all of her STI testing. She was not tested for herpes. Over time, she has felt better. Two months ago, she would have called her provoked and unprovoked pain level an 11/10 but now she is not having pain. She thinks she has been better for a couple of weeks. During the whole summer, she was unable to use tampons, which she has used for her periods since she was a teenager. She has been able to have intercourse only with some 2% Lidocaine gel applied in a small amount with a q-tip. She has no pain at other times. She has no itching at all. She only has pain, now, after intercourse. Pain with intercourse was never an issue prior to this experience.
Current pain symptoms on a scale from 0-10 at its worst: 2 out of 10
Symptoms of itching on a scale from 0-10 at its worst: 0 out of 10
Lifestyle issues: Non-contributory; she uses Dove soap for sensitive skin; no daily panty liners. She uses fragrance-free products; no wet wipes; clothing not too tight, no underwear to bed.
History and review of systems:
- Vulvovaginal history: Possible yeast and BV; no history of genital trauma or sexual abuse. STI testing negative.
- GYN history: Negative. Pap has been negative.
- Past and current medical conditions: None
- Past surgical history: None
- Review of associated systems:
- Urinary: Negative
- GI: Negative
- Musculoskeletal: Negative
- Dermatological: Negative
- Mental health: Negative
- Review of other systems: Negative
- Social history: Non-smoker, <3 drinks a week, no recreational drugs; exercises 5 hours a week at the gym
Medications:
- Multivitamins, one daily
- Tri-Sprintec OCP
Allergies:
- Rash from MMR vaccine
KEY POINTS FROM THE HISTORY:
- It is important to differentiate between dyspareunia from the time of first and subsequent attempts at intercourse (primary) and dyspareunia that occurs later, after a history of comfortable intercourse (secondary).
- Yeast might have been a precipitating factor, but after adequate treatment for yeast (and repeated negative culture results), a search for other causes should be made.
- Bacterial vaginosis does not cause pain.
Non-genital exam:
BMI: 20.97 kg/(m^2); vital signs within normal range.
GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Exam: well tolerated
Groin: normal skin color and texture
Mons pubis: normal, non-tender.
Labia majora: normal skin color and texture and normal anatomy.
Perineum: normal skin color and texture and normal anatomy.
Anus: normal skin color and texture and normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: normal architecture bilaterally, normal skin color and texture
Prepuce: normal and mobile.
Clitoris: visible.
Interlabial folds: normal skin color and texture and normal anatomy
Vestibule: non-tender to q-tip test, normal skin color and texture
Urethral meatus: normal size, normal location, no masses.
Vagina: well estrogenized, not inflamed and non-tender; Discharge: normal and scant.
Pelvic Floor: there is no hypertonicity on exam, but she may have situational hypertonicity with fear of pain with intercourse
Cervix: no lesions, no cervical motion tenderness.
Uterus: midline, mobile, smooth, non-tender, not enlarged.
Adnexa: not enlarged, no masses felt, non-tender.
Rectal: not indicated.


Microscopy:
Vaginal pH: 4.0
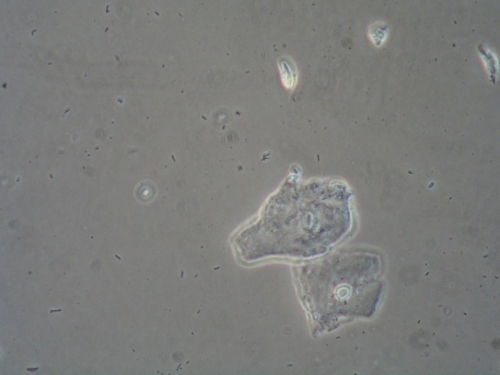
Wet prep: normal; one WBC per epithelial cell, no clue cells, no parabasal cells, no pathogens, normal lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM THE EXAM:
- A completely normal exam, with no replication of symptoms on Q-tip touch or palpation indicates that the symptoms have passed due to prior treatment (including elimination of irritants) or the passage of time.
- Yeast, BV, dermatosis are all ruled out with this exam. Vulvodynia is ruled out because pain is not currently present. Pelvic floor hypertonicity (situational) is not ruled out.
PRELIMINARY DIAGNOSIS:
- Episode of acute vulvovaginal pain following intercourse about three months ago, with prolonged symptoms of dyspareunia, now resolving
- Possible situational pelvic floor hypertonicity
- Possible pudendal nerve compression
- Possible unrecognized herpes infection
Plan:
Testing sent or ordered: Yeast culture and herpes titer for IgG type 1 and 2; Results: negative yeast culture; positive serum testing for herpes simplex type 1.
The patient, when told, said she may have had a cold sore “once.” She does not know about her boyfriend. She was called with the herpes result and told that the location of her Type 1 herpes cannot be known from the titer. She would have to look out for vulvar itching, irritation, skin breakdown in the vulvar area and come in for culture.
Education: General vulvar care, elimination of possible irritants, discussion about the possibility of situational pelvic floor hypertonicity causing the pain were all discussed and handouts given, including information on pelvic floor physical therapy.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days; continue daily to use topical Vaseline for moisturizing, comfort.
Treatment: A “wait and see” approach was taken after complete patient education. The patient was asked to keep a diary of symptoms, should they recur and be aware of triggers. She was taught about using Lidocaine 5% ointment, applying about ½ teaspoon to the vestibule (avoiding the clitoris) for at least 10-15 minutes prior to intercourse, wiping it off, and then applying a lubricant.
Return visit findings:
Three weeks later:
Yeast culture from the last visit was negative. The differential at that visit was previously unknown herpes simplex, situational pelvic floor hypertonicity, or pudendal nerve compression. The pt was told to do warm soaks and Vaseline and eliminate irritants, just for general vulvar care. She was asked to call with a flare of symptoms and was given 5% Lidocaine to use with intercourse if necessary. Her pain had started during and after sex (provoked pain) but had also been unprovoked, being present during the course of her day. Currently, the patient reports that she did well for a while and thought she was “over it,” but then, about a week ago, just when her period was over, she and her partner had intercourse and she again had excruciating pain with and after it that lasted for a few hours, with twinges continuing for days afterward. The pain was at a level of 7-8/10. The pain finally subsided a couple of days ago and they tried having sex again without incident. She did not have any pain during or afterward. She is comfortable today. She mentions that when she feels the pain (at 4-7:00 in the vestibule), she also has painful sensations in the gluteal cleft, up high, aiming toward the lower back.
The patient mentions, too, that she does yoga regularly and is a yoga instructor. She feels that she knows her body and how to relax it. She does not feel that she is tightening up in the pelvic floor with intercourse.
At the last visit, a herpes titer was done that was positive for Herpes Simplex type I. When she had the pain with sex last week, she did not see any skin breakdown in the vestibule.
On exam, the vestibule was non-tender to q-tip touch except at 6:00 where there was pain under the hymenal remnants. The skin was normal in color and texture. The rest of the exam was normal. There was no pelvic floor hypertonicity. PH and wet prep were normal.
Assessment:
Intermittent, acute, provoked, vulvar (vestibular) pain in the setting of a normal exam
Vestibular pain and flashes of erythema with Q-tip touch under the hymenal ring
Plan:
The patient was given the following handouts: Vulvodynia, My Partner has Vulvodynia, pudendal nerve compression, pelvic floor hypertonicity, and information on physiatry. A visit with a physiatrist familiar with pelvic floor disorders was recommended.
The patient, confident in her ability to control her pelvic floor, declined that appointment. She requested treatment with Amitriptyline, having had a friend with vulvodynia who had benefitted from it.
We gave her Amitriptyline, starting at 10 mg orally at bedtime, increasing every 5-7 days by 10 mg to a maximum of 100 mg. She was instructed to stop increasing the amount if she found herself comfortable at a lower dose. She was warned about side effects: dry mouth, constipation, sedation, weight gain, possible rapid heart rate, and asked to return in three months.
Ten months later:
The patient returned with flaring symptoms: itching, burning, dyspareunia, white clumpy discharge, and persistent provoked and unprovoked pain. She described a sensation “like pine needles, pricking from front to back.” Prior to this visit, she had used Monistat x 3 and taken Diflucan x 2. She was sure her symptoms were related to yeast. She reported having increased the Amitriptyline to 60 mg, staying on that for a while and feeling better, with resolution of her symptoms. She had, therefore, tapered down off of it a couple of months before. Exam was, again, normal, with pain at 6:00 in the vestibule only. No hypertonicity. pH and wet prep were normal, but she was given Diflucan 150 mg orally to take twice a week for two weeks for prevention of yeast. (Culture was negative.)
Assessment:
Neuropathic pain of unknown origin
Plan:
She was started on Gabapentin 100 mg orally at bedtime, to increase slowly, every 3-7 days by 100 mg to a maximum of 1,000 mg. She was informed of possible side effects, most commonly grogginess or feelings of “spaciness.”
Twelve and a half months later:
She described having acute pain just above the urethra, mostly with direct touch, and also feelings “like ants are biting her” from the top of the vulva (anterior commissure) to the anus. Yeast culture from the last visit was negative. The patient did not think this was related to hypertonicity. She had declined pelvic floor physical therapy. She had made an appointment with the physiatrist, however, for the next week. Was not able to have intercourse because of knife-like pain above the urethra. Gabapentin was of no help whatsoever.
On exam:
Interlabial folds: normal skin texture and normal anatomy; dark pink skin color. No pain with Q-tip touch.
Vestibule: The vestibule was non-tender to q-tip test, normal skin color and texture
Urethral meatus: normal size, normal location, no masses. Exquisite tenderness when touched with the Q-tip just above the urethral opening. No skin changes, normal color. No erythema.
Vagina: well estrogenized, not inflamed and non-tender; Discharge: normal and scant.
Pelvic Floor: there was no hypertonicity on exam; able to perform pelvic floor drop easily. Roomy pelvis. Some pain with downward palpation.
PH and wet prep: normal.
Assessment:
Flare in symptoms of vulvodynia (neuropathic pain), probably stimulated by yeast infection months before
Gabapentin not helpful
Plan:
Decrease the Gabapentin slowly, the same way she increased slowly originally. When down to 300 mg, start taking Amitriptyline again, 10 mg orally at bedtime, increasing slowly to a maximum of 100 mg.
See the physiatrist and get her opinion.
Use topical Lidocaine 5% up to 5 times a day to quell the ant-biting sensations.
Consider using vaginal Valium.
Fourteen months later:
The patient reported that the physiatrist found one hip higher than the other, with consequent rotation of the pelvis, probably contributing to her pain. She had her start pelvic floor physical therapy. She was using 50 mg of Amitriptyline and topical Lidocaine and was feeling a bit better, but continued to have periurethral pain with exam and was still not having intercourse. There was no hypertonicity in the levator muscles but there was pain on palpation in the obturator on the left (greater than the right), and higher, toward the piriformis muscle.
Environmental influences were discussed: the patient reported having onset of original symptoms starting soon after she took her current job which involves sitting for eight hours a day. Her symptoms are worse with sitting.
Assessment:
Provoked and unprovoked pain from pelvic obliquity and pelvic floor dysfunction with some improvement after initiation of pelvic floor physical therapy
Plan:
Continue increasing the Amitriptyline to 100 mg at bedtime.
Because yeast may have precipitated this episode, the patient was advised to take weekly Diflucan throughout the summer. She was asked to submit self-yeast cultures if symptomatic.
Discussed the importance of identifying triggers and taking action once they are identified. In the case of prolonged sitting, the patient can make it a habit to get up from her desk once an hour and move around. She can get a gel-filled cushion to put on her seat and have the ergonomics at her desk evaluated at work, etc. She should look at how tight her underpants are when she sits, etc.
Fifteen months later:
Phone call from patient: She was feeling a lot better, (pain down from 10/10 to 2/10), attributing her improvement to the pelvic floor physical therapy, Amitriptyline 70 mg at bedtime, and weekly Diflucan which she was about to stop. She was feeling very hopeful and was able to have comfortable intercourse again.
TEACHING POINTS:
- Neuropathic vulvar pain is mysterious in its tendency to persist past any possible initiating insult.
- The source of the pain must be sought out by a process of deductive reasoning. Potential physical causes should be treated.
- Residual pain, either primary or secondary, can be very difficult to treat. No one treatment is superior to another and, in some cases, treatment with medications is no better than treatment with placebo.
- It is important to not give up on the patient. Allied professionals can be very helpful in the evaluation and treatment process: physiatry, physical therapy, pain clinics, urogynecology, cognitive behavioral therapy, sex therapy, etc.
- It is important not to underestimate the impact of environmental factors, many of which are not considered to be variables at all by the patient.