#6: Itching
Age, G/P, relationship status, occupation: 48 year old, G0, married, elementary school teacher
Menstrual status: irregular menses
Contraceptive method: vasectomy
Sexuality status: Male partner; sexual intercourse is comfortable and enjoyable when itching is not prominent
Chief Complaint: Biopsy proven lichen sclerosus; clobetasol not helpful; she has itching.
Symptoms (HPI: history of present illness): Itching began three years ago; biopsy showed lichen sclerosus. She used clobetasol nightly for 30 days, then twice weekly. At first, it was helpful but now, itching has returned and is troublesome.
Lifestyle issues: washes with Ivory soap and uses Tide detergent
History and review of systems:
- Past and current medical conditions: sinusitis, frequent antibiotics, migraine headaches
- Past surgical history: tonsillectomy
- Review of associated systems:
- Urinary: denies
- GI: denies
- Musculoskeletal: arthritis in hip
- Dermatological: denies
- Review of other systems: migraines
Medications:
- Ibuprofen
- Topiramate
Allergies:
- None known
KEY POINTS FROM HISTORY:
- When treatment is not working, re-examine the diagnosis. In this case, a biopsy has been done to obtain an initial diagnosis, but if there is an ongoing concern, a review of the biopsy slide can be done.
- Make sure that the woman is using the medication properly, applying it in the correct area, in the correct amount.
- Bacteria, yeast, HSV, and resurfacing of HPV are always possible with steroid use.
Non-genital exam:
BMI: 30.44 kg/(m^2). Vital signs within normal range GENERAL: overweight female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Exam: well tolerated
Mons pubis: normal, non-tender.
Labia majora: normal anatomy but the skin is erythematous and crinkled down to buttocks, itchy to touch.
Perineum: erythematous and fissured, itchy to touch.
Anus: normal skin color and texture and normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: normal architecture bilaterally, erythematous, inflamed, and itchy.
Prepuce: normal and mobile, but erythematous.
Clitoris: visible.
Interlabial folds: erythematous, itchy
Vestibule: itchy to Q-tip touch test, erythematous
Urethral meatus: normal size, normal location, no masses.
Vagina: inflamed and erythematous; Discharge: normal and scant.
Pelvic Floor: no hypertonicity
Cervix: no lesions, no cervical motion tenderness.
Uterus: midline, mobile, smooth, non-tender, not enlarged.
Adnexa: not enlarged, no masses felt, non-tender.
Rectal: not indicated.

Microscopy:
Vaginal pH: 4.4
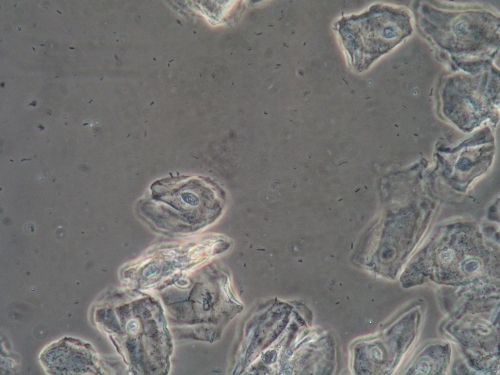
Wet prep: normal epithelial cells; one WBC per epithelial cell, no clue cells, no parabasal cells, no pathogens, normal lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM THE EXAM:
- Extensive erythema can indicate yeast even without it being visible on microscopy. Erythema may also indicate super-imposed bacterial infection or contact dermatitis. For yeast, look for tiny, satellite, red papules or pustules on the outer edges of the erythema.
- With erythema in the case of a treated dermatosis, steroid rosacea must also be considered.
- In this case, the vagina was also inflamed, (even though the wet prep was normal), whereas lichen sclerosus does not cause that.
PRELIMINARY DIAGNOSIS:
- Lichen sclerosus with secondary yeast, even though microscopy is negative
Plan:
Testing sent or ordered: Vaginal yeast culture Result: positive for C. Albicans.
Bacterial culture of skin: Result: normal flora.
Education: General vulvar care; handout on the use of steroids in vulvar care, handout on yeast. Patient taught to be on the lookout for yeast and call for increased itching.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days.
Treatment: Fluconazole 150 mg orally, day one and day three, then weekly. Continue clobetasol 0.05% in a thin film to the skin affected by lichen sclerosus, twice weekly.
Return visit findings: Itching came into control and was kept in remission with weekly fluconazole for four months, then spaced out to every other week, then stopped. The skin reverted to a normal appearance.
TEACHING POINTS:
- Microscopy is not helpful for Candida albicans ~ 40% of the time.
- Yeast culture with visits is a valuable adjunct.