#4: Localized, provoked pain
Age, G/P, relationship status, occupation: 24 year old, G0, single, student
Menstrual status: regular
Contraceptive method: OCP for periods
Sexuality status: partners with men, never sexually active, not in a relationship.
Chief Complaint: localized, provoked vulvar pain
Symptoms (HPI): The patient states that she was first aware of her vulvar pain as a teenager when she tried to use a tampon. She felt like she was encountering so much resistance that, “it felt like there was not a hole there and afterwards I had burning.” The patient has been followed by her gynecologist for this pain and a number of therapies have been instituted for her including topical lidocaine, which she found helpful, pelvic floor physical therapy, which she found helpful, and dilator therapy. She ended up stopping her pelvic floor physical therapy after six visits, three years ago, because she got a job and could no longer make the appointments. Vaginal valium and Percocet were prescribed for her, but she never started them. She was given an estradiol and testosterone topical gel in methylcellulose base and she used that twice daily for a year. She did not find it particularly helpful and stopped it three years ago. She has had vestibulectomy recommended to her.
Lifestyle issues: no environmental irritants
History:
- Past and current medical conditions: negative
- Past surgical history: none
- Associated review of systems:
- Urinary: overactive bladder symptoms with urinary frequency and nocturia and difficulty emptying her bladder completely. She has seen a urologist and was given oxybutynin, but found that it made it harder for her to urinate
GI: constipation, diarrhea, abdominal pain - Musculoskeletal: negative
- Dermatological: negative
- Urinary: overactive bladder symptoms with urinary frequency and nocturia and difficulty emptying her bladder completely. She has seen a urologist and was given oxybutynin, but found that it made it harder for her to urinate
- Other review of systems: negative
Medications:
- OCP
Allergies:
- Codeine, erythromycin, penicillin, sulfa
TEACHING POINTS FROM THE HISTORY:
- She describes provoked pain in the vestibule with no prior sexual intercourse.
- There are urinary and bowel symptoms that may be aggravating the pelvic floor.
- Searching for the source of the pain is the goal of the examination.
Non-genital exam
BMI: 20.25 kg/(m^2); vital signs within normal range.
GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Exam: well tolerated despite pain
Mons pubis: normal, non-tender.
Groin: normal skin color and texture
Labia majora: normal skin color and texture and normal anatomy.
Perineum: normal color and texture, painful to touch.
Anus: normal anatomy, normal color and texture.
Bulbocavernosus reflex and anal wink present.
Labia minora: flattened bilaterally posteriorly, normal color and texture.
Prepuce: normal and mobile; normal color.
Clitoris: visible.
Interlabial folds: normal color and texture
Vestibule: tender to q-tip touch test diffusely from 3 to 9:00 and onto the perineal tissue; erythematous.
Urethral meatus: normal size, normal location, no masses.
Vagina: inflamed and tender; Discharge: moderate amount, yellow.
Pelvic Floor: hypertonicity present on exam with diffuse tenderness in the pelvic floor muscles
Cervix: no lesions, no cervical motion tenderness.
Uterus: midline, mobile, smooth, non-tender, not enlarged.
Adnexa: not enlarged, no masses felt, non-tender.
Rectal: not indicated.

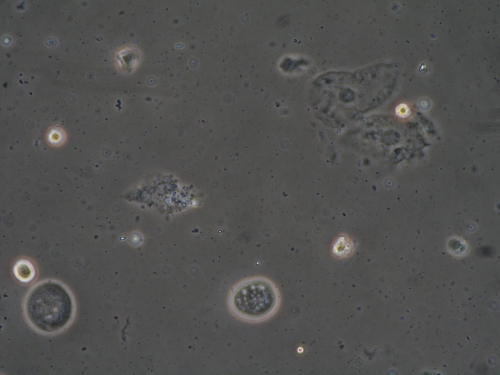
Microscopy:
Vaginal pH: 4.4
Wet prep: normal epithelial cells; 2-3 WBC per epithelial cell, no clue cells, 1% parabasal cells, no pathogens, few lactobacilli
KOH: negative whiff and negative for pseudohyphae or spores
KEY POINTS FROM THE EXAM:
- Although the pH was in the normal range, the presence of parabasal cells, along with increased numbers of WBC’s and only a few lactobacilli, led to the diagnosis of DIV.
- Classical DIV presents with an elevated pH, many WBC’s, and an absence of lactobacilli. This less classical, less obvious form has not been discussed in the literature.
PRELIMINARY DIAGNOSIS:
- Desquamative inflammatory vaginitis (DIV)
- Secondary pelvic floor dysfunction
Plan:
Testing sent or ordered: Yeast culture and trichomonas culture Results: both negative
Education: Discussion and handouts on DIV, pelvic floor impact on vulvar pain, pelvic floor physical therapy
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days.
Treatment: Compounded hydrocortisone 100 mg suppositories inserted into the vagina nightly x 14 days then Monday, Wednesday, Friday; physical therapy to the pelvic floor.
Return visit findings:
Eight weeks later:
She was much improved. Erythema regressed; there was minimal allodynia, good pelvic floor drop. pH 4.4, no parabasals, no yeast forms, 0-1 WBC’s per epithelial cell, moderate lactobacilli. Vaginal hydrocortisone was dropped to once weekly. She steadily improved, but effort to taper off hydrocortisone after 16 weeks led to resumption of symptoms. After another 12 weeks of hydrocortisone 100 mg Monday, Wednesday, Friday, she was able to switch to Anusol HC (25 mg) suppositories, used vaginally twice weekly. Her urinary symptoms resolved.
TEACHING POINTS:
- Localized provoked pain arose from inflammatory vaginitis, which led to pelvic floor hypertonicity.
- She needed treatment of the inflammation as well as treatment of the pelvic floor.
- Urinary symptoms were probably related to periurethral irritation.
- Inflammatory vaginitis is often chronic, coming and going in an unpredictable fashion, and requires chronic management.