#10: Itching and dyspareunia
Age, G/P, relationship status, occupation: 46 year old G2 P2 (both Cesarean sections) married homemaker
Menstrual status: Regular menstrual periods
Contraceptive method: tubal ligation
Sexuality status: Male partner; intercourse has become more and more difficult due to pain
Chief complaint: “frequent yeast infections that never seem to go away;” itching.
Symptoms (HPI: history of present illness): The patient was treated for Hodgkin’s lymphoma five years ago with chemo and radiation. She also had to take antibiotics at that time. She thinks that was when her symptoms started. She had itching, burning, and rawness that was very uncomfortable. Most of the symptoms are on the outside of her vulva rather than on the inside, but she also has had terrible pain and burning with intercourse. She complains, as well, of “pain in the lower stomach and right side with cramping and bloating, at least five out of seven days a week.” If she rinses her skin off, she feels better temporarily. Nothing else helps much. She has been given fluconazole and over the counter creams, including Betamethasone with Clotrimazole 0.05%/1%, for yeast which also help temporarily. She went without a period for some time after being treated for the Hodgkin’s but now her periods are regular again.
Lifestyle issues: Tide, Era, and Fab detergent, Downy fabric softener, Clorox bleach, Always brand sanitary pads
History and review of systems:
- Vulvovaginal history: Yeast infections, bacterial vaginosois; no history of genital injury or trauma; no history of sexual abuse or assault.
- GYN history: no previous abnormal Paps; Right oophorectomy and salpingectomy for torsion. Large left ovarian cystectomy.
- Past and current medical conditions: Hodgkin’s lymphoma, hypothyroidism, anxiety, and depression
- Past surgical history: R oophorectomy and salpingectomy, L ovarian cystectomy, tubal ligation, Cesarean section x 2.
- Review of associated systems:
- Urinary: History of urgency and leakage of urine
- GI: History of constipation, reflux, and abdominal pain
- Musculoskeletal: Negative
- Dermatological: History of thrush in her mouth
- Mental health: History of depression, anxiety, high-stress, perceived poor health, lack of emotional support, difficulty in relationship and distress about vulvovaginal condition
- Review of other systems: Negative
- Social history: smokes nine packs of cigarettes a week, no alcohol, no recreational drugs, no exercise.
Medications:
- Levothyroxine 75 mcg daily
- Celexa 40 mg daily
- Omeprazole 20 mg daily
Allergies:
- Sulfa
- Levofloxacin
KEY POINTS FROM HISTORY:
- The history does point to yeast, although she had frequent treatment; one might assume she would have been cured.
- Cancer treatment can make people more susceptible to recurrent yeast, probably because of changes to the immune system.
Non-genital exam:
BMI: 24.46 kg/m2
GENERAL: well-nourished female. Orientation and affect normal. MOUTH: There are no oral or gingival lesions. SKIN: Her skin is clear without lesions. NAILS: normal. NECK: supple without masses; RESPIRATORY: normal chest excursions ABDOMEN: The abdomen is soft, non-tender without mass, organomegaly, or inguinal hernia. There are no inguinal lesions or nodes. Femoral pulses are normal. There is no tenderness to palpation over the bladder.
Genital exam and symptom mapping:
Exam: well tolerated
Mons pubis: normal, non-tender; anterior commissure: erythematous
Groin: normal skin color and texture and normal anatomy
Labia majora: normal skin color and texture and normal anatomy.
Perineum: erythematous.
Anus: normal skin color and texture and normal anatomy.
Bulbocavernosus reflex and anal wink present.
Labia minora: normal architecture bilaterally, erythematous and smooth; itchy to touch
Prepuce: normal and mobile, but puffy.
Clitoris: visible.
Interlabial folds: glossy, erythematous, and excoriated, itchy
Vestibule: burning with q-tip touch test, erythematous; itchy
Urinary meatus: normal size, normal location, no masses, no tenderness.
Vagina: well estrogenized, erythematous and non-tender; Discharge: scant and white.
Pelvic Floor: there is no hypertonicity.
Cervix: no lesions, no cervical motion tenderness.
Uterus: midline, mobile, smooth, non-tender, not enlarged.
Adnexa: right side absent. Left side normal, mobile, slightly rounded in shape, non-tender.
Rectal: not indicated.

Microscopy:
Vaginal pH: 4.0
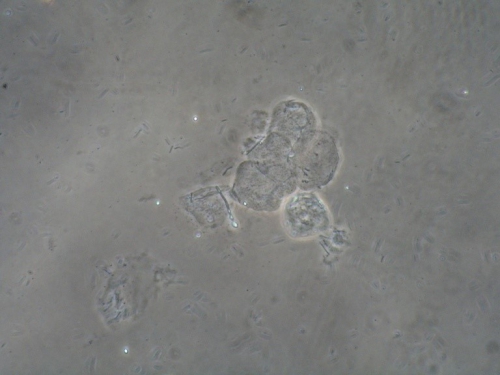
Wet prep and KOH: normal epithelial cells, parabasal cells: 0%, clue cells absent, pseudohyphae present, 1 WBCs per epithelial cell, many lactobacilli present and trichomonas absent
KOH: negative whiff and positive for pseudohyphae
KEY POINTS FROM EXAM:
- Excoriations (and sometimes broken hairs) are indicative of scratching and may be characteristic of lichen simplex chronicus, especially if lichenification is also present.
- The patient’s reddened, smooth, and glossy skin indicates trauma, whether from yeast itself or from rubbing to soothe the itching.
- Burning is caused by the presence of yeast and the skin breaking down with rubbing.
PRELIMINARY DIAGNOSIS:
- Lichen simplex chronicus
- Candidiasis
- The patient also had on-going abdominal pain, including in the LLQ and was advised to follow up with her own doctors about this. On PET scan in follow up to the Hodgkin’s, they saw a “tiny” lesion in the area of her pain and she is worried she might have a metastasis. She was told she needs no further scans. I advised her to call her oncologist, as well, to discuss the symptoms.
Plan:
Testing sent or ordered: Yeast culture; Results: positive for C. Albicans
Education: Handouts given: general vulvar care, lichen simplex chronicus, yeast infection. Educated about the nature of LSC so she understood the importance of stopping scratching in order to heal. Informed that the condition may recur, given circumstances that promote it. Instructed to avoid irritants, including those that she might not recognize as such: thongs, tight clothing, jeans, underwear to bed, scrubbing of the skin, use of daily panty liners, etc.
Restoration of the epithelial barrier: soak (5-10 minutes, tepid water) and seal with Vaseline twice daily for seven days. Then should use Vaseline as a moisturizer whenever possible.
Treatment: Betamethasone diproprionate 0.05% with Clotrimazaole 1% ointment (about the size of 1/2 a pea) spread over the itchy parts of the skin in a very thin film, using the smallest amount of ointment that will spread, twice a day for 14 days, then once a day for 14 days, then twice weekly if still needed. She was given topical Lidocaine 5%, a small amount up to 5 times a day, to help subdue the itching and burning so that she would be less likely scratch. She was warned that Lidocaine may burn initially when first applied, then numb the skin.
To treat the yeast, she was given a 7 day course of Clotrimazole vaginal cream followed by using one applicator full twice weekly.
Return visit findings:
One and a half months later:
Culture had confirmed Candida Albicans and she was treated. The patient was symptom-free. Still using the topical Betamethasone/Clotrimazole and the twice-weekly applicator of Clotrimazole. Intercourse was much more comfortable.
Since her last visit, she was diagnosed with a hemorrhagic ovarian cyst on the left side for which she planned surgery. She had also had an experience with visual disturbance: she lost peripheral vision and saw blinking lights. She had a brain MRI which was normal. They are thinking she had a migraine equivalent.
On exam, the skin was clear. However, there was a tiny brown line at the base of the vestibule, immediately above the perineum that could not have been caused by childbirth (two C/S). A biopsy was offered and accepted. The biopsy result was consistent with chronic inflammation and lichen simplex chronicus.
The patient was instructed in tapering the medications but having early awareness of symptoms to intervene before the situation gets out of hand. We also discussed prevention.

TEACHING POINTS:
- LSC (lichen simplex chronicus) is an eczema-like skin condition caused by the itching from a yeast infection, from eczema, or from an environmental irritant and then made worse by scratching so that it becomes its own condition. To heal, it is essential to stop scratching and rubbing the skin, including at night.
- If yeast is chronic or persistent, lichen simplex chronicus may be secondary to it, caused by scratching.
- Itching may be present, even if the yeast is taken care of, because of the lichen simplex.
- In this patient’s situation, we gave her Clotrimazole for the yeast, rather than Diflucan, because she was taking Celexa. There are many drug-to-drug interactions with Diflucan (fluconazole) and a judgment must be made about which medication to recommend when treating yeast.