Introduction
Edema is a common feature of many vulvar conditions and varies from barely perceptible to massive.
Fluid accumulation from either plasma or the lymphatic system in the loose areolar tissue of the vulva results in vulvar edema. Fluid from the plasma is usually acute and transient and is termed angioedema. Fluid from lymphatic origin persists chronically and is termed lymphedema.
Massive lymphedema is often called elephantiasis. Swelling can be caused by a single condition as outlined below, or by combination of inflammation, infiltration, lymphatic disruption or obliteration. If there is disease involving vascular damage, angioedema may transition into lymphedema, blurring the classification.1
Classification of Edema
-
I. Inflammatory Angioedema
- A. Allergic and immune reactions
- 1. Angioedema with or without urticaria
- 2. Allergic IgE medicated contact dermatitis, or non-IgE medicated
- a. Latex
- b. Seminal plasma allergy
- c. Ingested foods
- B. Infection
- 1. Streptococcal cellulitis
- 2. Candidiasis
- 3. Necrotizing fasciitis
- 4. Rare infections
- a. Tuberculosis,
- b. Actinomycosis,
- c. Granuloma Inguinale,
- d. Amebiasis,
- e. Blastomycosis,
- f. Schistosomiasis
- C. Inflammation
- 1. Granulomatous inflammation
- a. Crohn disease
- b. Melkerson-Rosenthal type syndrome
- c. Sarcoidosis
- 2. Other inflammation
- a. Acute trauma.
- b. Amyloidosis
- c. Infiltrative neoplasm
- d. Hidradenitis
- 1. Granulomatous inflammation
- A. Allergic and immune reactions
-
II. Obstructive lymphedema
- A. Congenital
- 1. Milroy’s disease
- 2. Lymphangioma
- B. Acquired
- 1. Lymphangiectasia/acquired lymphangiomas
- 2. Infection with secondary lymphatic damage
- a. Recurrent cellulitis from streptococcus
- b. Crohn’s -secondary lymphatic obstruction
- c. Hidradenitis- secondary lymphatic
- d. Other rare obstructive infections
- i. Lymphogranuloma venereum
- ii. Filariasis,
- iii. Granuloma Inguinale,
- A. Congenital
-
III. Physical lymphatic obstruction from mass, tumor, or destructive process
- A. Pregnancy
- B. Pelvic or local trauma
- C. Pelvic tumor
- D. Post-radiation scarring
- E. Congestive heart failure
-
IV. Metabolic causes
- A. Obesity
- B. Renal failure
- C. Hepatic failure
Epidemiology
Information is largely limited to case reports; incidence and epidemiology are not established in many cases. Clinical experience has taught us that in a woman with lymphedema of the lower limbs, vulvar lymphedema is a real possibility.
Latex allergy (which may cause edema) occurs in about 4% of health care workers, and about 1% of the general public.2
Etiology
Inflammatory, infectious, obstructive, or metabolic processes allow fluid from the plasma or lymphatics to accumulate in lax vulvar tissue.
Symptoms and clinical features
Both angioedema and lymphedema may be asymptomatic.
However, the labia majora and labia minora can become swollen enough to extend up to six inches from their bases. Women describe a dragging, heavy, bursting sensation or aching in the vulva. Sudden distention that may occur with either angioedema or lymphedema, may yield pain. With allergic reaction, itching is present. With infection, irritation and soreness are features. Wide fissures and erosions are painful. The skin may be thickened and dry, with flaking.
Leakage of clear fluid from lymphoceles on the vulvar skin may necessitate use of pads to absorb the fluid, and increases risk of infection. Proper treatment of lymphedema is necessary to stop this leakage.
Sexual desire and function are inhibited by the physical appearance, discomfort and/or pain, and drainage.
With both types of edema, the clinical feature of tissue distention of the vulva is present.
Angioedema from allergic and immune reactions develops over minutes to hours and evolves over hours to days. It is often pitting edema. It resolves and the skin returns to its normal shape and appearance after the episode is over. With angioedema, urticaria may or may not be present. IgE mediated reactions can lead to anaphylaxis.
Acute vulvar angioedema is usually an allergic reaction to topical or systemic ingestion to which a woman has been sensitized by prior exposure. Semen (Annotation J: Lifestyle issues) and latex in condoms, diaphragms, and gloves are the most common IgE mediated allergens.3 Finding the antigenic agent may be a challenge since it may be a seemingly harmless item like a fragrant after-shave her partner uses.4 (Vulvar Atlas: Contact dermatitis, irritant and allergic). Clinical presentations vary but may include contact urticaria, coryza, conjunctivitis, stinging or burning, edema, and anaphylaxis.
Erythema in a contact pattern may be seen with allergic contact dermatitis. Vulvar itching and erythema may appear after ingestion of allergens such as shellfish and peanuts.
Angioedema from infection with lymphatic blockage
Recurrent streptococcal cellulitis can cause progressive edema and vulvar distortion, redness and irritation, itching or burning. There are usually no systemic signs.
Candida often produces fissures and small erosions.

Genital edema with chills, fever, and elevated white count accompanies necrotizing fasciitis.
Rare infections have links below.
Blastomycosis – all uncommon- have unique skin findings.
Schistosomiasis (bilharzia) produces progressive and relapsing vulvar swelling, painful or painless ulceration, nodularity, pruritus and a hypertrophic clitoris.5 The eggs of the trematode parasitic worm Schistosoma hematobium often spread from the blood to pelvic organs and the bladder prior to manifesting on the vulva.6
Inflammation
Granulomatous inflammation: Crohn disease is separately discussed. (Crohn disease in Atlas)
Melerson-Rosenthal type syndrome features edema of the lower extremities and vulvar edema similar to lymphedema.
Other inflammatory conditions which cause edema:
Acute trauma (trauma in Atlas)
Amyloidosis can masquerade as an eczematous process covering the vulva.7
Infiltrating neoplasms cause inflammation and edema.
Hidradenitis is separately discussed. (Hidradenitis suppurativa in Atlas).
Obstructive Lymphedema
Lymphedema may be congenital (primary).
Congenital lymphedema
Milroy disease represents a rare congenital abnormality with lack of development of the lymph vessels8 in the lower portion of the body. The disease affects the lower extremities; rarely, vulvar edema occurs.
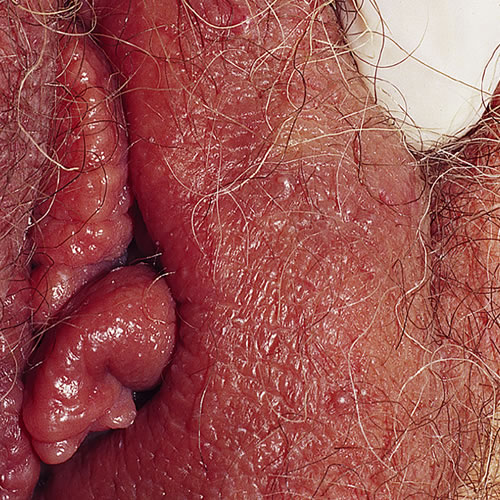
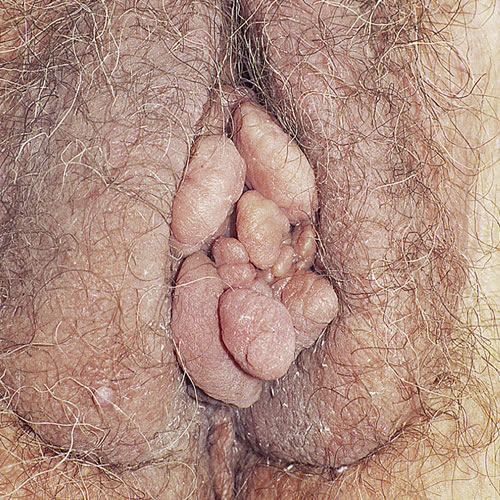
Lymphangioma, a rare congenital abnormality in the reticular dermis, prevents connection of lymphatic sacs to lymph vessels. (lymphangioma). Lesions may occur in any region. On the vulva, lesions appear as a localized cluster of small, superficial vesicular sacs containing clear, milky, or bloody fluid. Lymphangioma circumscriptum may be associated with cavernous lymphangioma lying deep to the clusters. Acquired lymphedema arises when infection or other obstruction of the lymphatics occurs, or from tumor, radiation, or surgery. This edema is firm to palpation and pits less easily. It can cause the vulva to acquire a verrucous appearance sometimes mistaken for genital warts.9

An acquired form of lymphangioma circumscriptum called lymphangiectasia occurs after repeated bacterial infection has led to chronic edema. It is often seen in cutaneous Crohn disease.

Infection with secondary lymphatic damage
Recurrent cellulitis can lead to repeated lymphatic damage, resulting in stasis. Immune response is reduced,10 and infection recurs.
With further cellulitis, there is more destruction of lymphatics leading to a vicious cycle. The cutaneous infection appears to arise spontaneously without injury or a break in the overlying skin. Streptococcus is the primary pathogen. Symptoms may not occur, or may be mild so that patients are often unaware that the edematous area is infected. There is also no reliable means of obtaining cultures. Protracted antibiotic treatment is often necessary.11
Crohn disease (Crohn disease in the Atlas) and hidradenitis (hidradenitis suppurativa in the Atlas) may also create secondary lymphatic blockage.
Other rare infections below have links with complete information,
Acute trauma can result in genital edema and is usually recognizable by history. Lengthy bicycle riding is a common cause.12 Hair coiling strangulation, most often of the clitoris will produce massive pain and edema.
Tumor or neoplasm may produce inflammation, vascular involvement, or lymphatic obstruction resulting in vulvar edema. Ruling out pelvic or vulvar tumor is always an important part of diagnosis.
Irradiation of malignant vulvar or pelvic tumors usually results in a degree of secondary cutaneous reaction, either acutely or chronically. Acute radiation vulvitis occurs at the end of the course of radiation. There is edema with violaceous discoloration, pain, burning and occasionally frank bullae, and necrosis.13
In late radiodermatitis the changes are seen years after radiation therapy. The vulvar skin is thinned, whitened, scarred, and shows extensive telangiectasia.14

Other edema
Edema related to venous congestion may be seen in the obese. It is also thought that groin pressure from the enlarged abdomen contributes. Edema also results from high output failure due to low protein and venous congestion in congestive heart failure, renal failure, and liver disease.
Edema in pregnancy is related to both venous and lymphatic obstruction from the growing fetus. Edema related to pregnancy, especially pregnancy associated with preeclampsia, may occur through increased hydrostatic pressure. Edema is also frequently encountered in the postpartum period, and may persist for months. Vulvar edema occurring in immediate postpartum period has been reported to cause maternal deaths due to vascular collapse in six patients with an 80% mortality rate.15 Vulvar edema is also reported in the ovarian hyperstimulation syndrome as a result of decreased oncotic pressure and increased hydrostatic pressure.16
Diagnosis
History is key. The pregnant patient, the patient with pelvic surgery or radiation, recent trauma, CHF, renal or hepatic failure, gives vital information. Ask about allergies, eczema and asthma (demonstrating atopy), then listen for recent contact with known allergens or irritants. In the atopic patient with eczematous dermatitis, scratching can lead to secondary infection, cellulitis, and edema. Ask about a history or family history of Crohn disease and order a colonoscopy. Ask about a history of acne, axillary and submammary lesions, cysts, or family history of “boils.” Ask about a history of sarcoidosis.
Consult the referenced websites for historical information regarding rare infections. Ask for history of previous malignancy and always consider imaging with ultrasound, CT, or MRI to rule out tumor. Consider necrotizing fasciitis in a patient who appears toxic.
Do a careful evaluation of the skin. Look for fissures and excoriations to suggest scratching, pitting and scars and nodules in the groin from hidradenitis.
Pathology/laboratory findings
Biopsy of individual lesions, as well as of generalized edema, is helpful to look for granulomas. Cultures for yeast, bacteria, and virus are necessary. Histopathology will vary with diagnosis. Intercellular spongiosis will always be present. Lymphocytes and eosinophils are present with allergic dermatitis, granulomatous changes with granulomatous inflammation, positive gram stains for bacteria, positive PAS stains for fungi. With lymphatic disease, there are dilated thin-walled lymphatic vessels. For rare skin conditions, links provided include histopathology. If tumor or neoplasm is present the pathology, likewise, will vary.
Differential diagnosis
Infection, neoplasm, congenital lymphatic anomaly, trauma, inflammatory and metabolic disorders.
Treatment/management
A work-up to discern the cause of the edema is essential.
Angioedema is treated according to cause. The offending allergen must be withdrawn. 25-50 mg orally of Benadryl is helpful; occasionally a course of prednisone may be necessary.
Seminal plasma allergy is described in Annotation J: Lifestyle issues.
Recurrent streptococcal cellulitis is treated with antibiotics such as penicillin in the non-allergic (penicillin V potassium 300-500 mg orally four times daily for six weeks, tapering to one dose daily over three to six months. Erythromycin 500 mg every six hours for seven to ten days, or longer if needed. Sometimes a course of oral prednisone may be necessary
Candida treatment is discussed in Annotation P: Vaginal secretions, pH, microscopy, and cultures, section on Candida Albicans.
For angioedema of infectious etiology, see the links below.
Schistosomiasis
For angioedema of obstructive etiology, see the links below.
Crohn disease (Crohn disease in Atlas)
Melkerson-Rosenthal type syndrome is treated with intralesional injections of triamcinolone acetonide (Kenalog)®; these may or may not be accompanied with oral anti-inflammatory agents including dapsone, metronidazole or methotrexate.17
Lymphedema
Although numerous surgical and pharmacological interventions have been studied for secondary lymphedema, there is no specific review of vulvar therapy. Most lymphedema patients are treated in a comparable fashion. To date, no lymphedema treatment offers unequivocal benefit and some have deleterious side effects. Multimodal therapy – the combination of manual lymphatic drainage (MLD), remedial exercises, skin care, and compressive garments – has been shown to be effective.18
MLD is a highly specialized massage technique designed to enhance the sequestration and transport of lymph. Specialized stroke duration, orientation, pressure, and sequence are utilized with the goal of directing congested lymph through residual functioning channels into intact nodal basis.19 A therapist may be found through a lymphedema clinic located by contacting the gynecology department of a teaching institution or the American Society of Physical Therapists. Support garments used for vulvar varicosities are helpful. V Brace® by Fembrace and V Supporter® By Prenatal Cradle are worn day and night. Biker shorts with compression in the crotch Elvarex® from Jobst can be helpful. A woman needs to make sure that when she is measured for the shorts the therapist knows that she needs compression in the crotch.
Skin care includes daily bathing with an antibacterial soap (an exception to our suggestion of Dove® soap) and drying the area afterwards is very important to reduce the likelihood of infections. Regular moisturizing with an aqueous cream such as CereVe will deter dryness and flaking skin and keep the area soft. As this area is prone to fungal infections and cellulitis, regular self-skin checks will enable the patient to detect any early signs of inflammation. If an infection occurs, prompt anti-fungal or antibiotic treatment is required. If a patient suffers from recurring cellulitis episodes, then long-term prophylactic antibiotics may be required.
Exercise. A specific form of exercise for vulvar edema is pelvic floor exercise. Together with abdominal exercises and diaphragmatic breathing, pelvic floor exercises can help in reducing the edema. A lymphedema specialist or physiotherapist can instruct in these
Other information as well as a link to lymphedema support groups is available at http://www.lymphedemapeople.com.
For chronic conditions unresponsive to medical therapy, a surgical procedure may be necessary. Excisional techniques are most effective for severe forms of the disease. In select cases, subcutaneous tissue excision with preservation of the overlying skin is appropriate. However, for most patients, excision of the skin and subcutaneous tissue with split-thickness grafting is most effective.20
Milroy’s disease and lymphangioma circumscriptum, lymphangiectasia
Pregnancy related edema is treated with supportive care. Avoiding prolonged standing or sitting is important. Bed rest may be helpful. Compression garments and therapeutic massage with a physical therapist trained in lymphedema treatment are key. Vulvar edema from ovarian hyperstimulation will resolve as ovarian function corrects.
Trauma related edema will resolve with appropriate treatment. (Trauma). Properly protected gel or ice packs are helpful.
Radiation lymphedema is discussed in Annotation O: The vaginal epithelium.
References
- Lynch PJ, Skin-colored lesions. In: Edwards, L, Lynch PJ, eds. Genital Dermatology Atlas, 2nd ed. Philadelphia, Wolters Kluwer/Lippincott Williams & Wilkins, 2011. 222.
- Bousquet J, Flahault A, Vandenplas O, et al. Natural rubber latex allergy among health care workers: a systematic review of the literature. J Allergy Clin Immunol, 2006; 118:447-454.
- Lynch PJ, Skin-colored lesions. In: Edwards, L, Lynch PJ, eds. Genital Dermatology Atlas, 2nd ed. Philadelphia, Wolters Kluwer/Lippincott Williams & Wilkins, 2011. 222.
- Margesson LJ, Contact dermatitis of the vulva. In: Edwards, L, ed. Dermatol Ther 2004; 17:20-27.
- Crump, J.A., Murdoch, D.R., Chambers, S.T., Aickin, D.R., Hunter, L.A. Female genital schistosomiasis. J. Travel. Med. 2000; 7: 30–32.
- Poggensee G, Feldmeir H. Feamle genital schistosomiasis: facts and hypotheses. Acta Trop 2001; 79(1):193-210.
- Konishi A, Fukuoka M, Nishimura Y. Primary localized cutaneous amyloidosis with unusual clinical features in a patient with Sjögren’s syndrome. J Dermatol, 2007; 34(6):394-396.
- Ghaemmaghami F, Zarchi M, Mousavi A. Surgical management of primary vulvar lymphangioma circumscriptum and postradiation: case series and review of the literature. J Minim Invasive Gynecol, 2008; 15(2):205-208.
- Horowitz IR, Monaghan JM, McKay M. Vulvar tumors. In: Black M, McKay M, Braude P, Vaughan Jones S, Margesson L, eds. Obstetric and Gynecologic Dermatology, 2nd ed. London, Mosby International Limited, 2002. 179.
- Keeley VL. Lymphedema and cellulitis: chicken or egg? Br J Dermatol, 2008; 158:1175-6.
- Lynch PJ, Skin-colored lesions. In: Edwards, L, Lynch PJ, eds. Genital Dermatology Atlas, 2nd ed. Philadelphia, Wolters Kluwer/Lippincott Williams & Wilkins, 2011. 224.
- Baeyens L, Vermeesch E, Bourgeois P. Bicyclist’s vulva: observational study. Br Med J. 2002; 325:138.
- Fisher BK, Margesson LJ. Genital Skin Disorders. St Louis, Mosby, 1998, 123.
- Fisher BK, Margesson LJ. Genital Skin Disorders. St Louis, Mosby, 1998, 123.
- Finkler NJ, Safon LE, Ryan KJ. Bilateral postpartum vulvar edema associated with maternal death. Am J Obstet Gynecol. 1987; 156:1188-1189.
- Luxman D, Cohen JR, Gordon D., et al. Unilateral edema associated with severe ovarian hyperstimulation syndrome. J Reprod Med. 1996; 4: 771-774.
- Sobjanek M. Wlodarkiewicz A, Zelazny I, et al. Successful treatment of Melkerson-Rosenthal syndrome with dapsone and triamcinolone injections. J Eur Acad Dermatol Venereol. 2008; 22:1028-1029.
- Cheville AL, McGarvery CL, Petrek JA, Russo SA, Taylor ME, Thiadens SRJ. Lymphedema management. Semin Rad Oncol. 2003; 13(3):290-301.
- Cheville AL, McGarvery CL, Petrek JA, Russo SA, Taylor ME, Thiadens SRJ. Lymphedema management. Semin Rad Oncol. 2003; 13(3):290-301.
- McDougal WS. Lymphedema of the external genitalia. J Urol. 2003 Sep;170(3):711-716.