Introduction
Cellulitis1 is an acute, spreading, subcutaneous, bacterial infection causing areas of hot, red, tender skin. The organism enters through a small abrasion or split in the skin and then spreads.
Erysipelas is a superficial form of cellulitis.
Epidemiology
Both are more prevalent in patients with diabetes or chronic lymphedema. While cellulitis and erysipelas are not common vulvar problems, they need to be considered in patients with extensive vulvar dermatitis or dermatosis that is secondarily infected.
Etiology
Group A ß-hemolytic streptococci (GABHS) and Staphylococcus aureus are the organisms most likely to be found in cellulitis. Almost all erysipelas is caused by Group A beta hemolytic streptococci (Streptococcus pyognenes).

With repeated infection in diseases such as hidradenitis suppurativa, Crohn disease, or repeatedly infected lichen simplex chronicus, lymphatic drainage may be significantly compromised. There is always a degree of residual lymphedema predisposing to recurrent episodes of cellulitis.
Symptoms and clinical features
Cellulitis can be subtle when it involves the vulva, with only slight erythema, tenderness, soreness and a mild fever.

If involvement is extensive, there may be intense tenderness, fever, and malaise.

The labia may be red and warm or hot. In the perineum, sharply demarcated, red, indurated, plaques may occur and gradually spread. In severe cases, there are sometimes bullae and erosions.
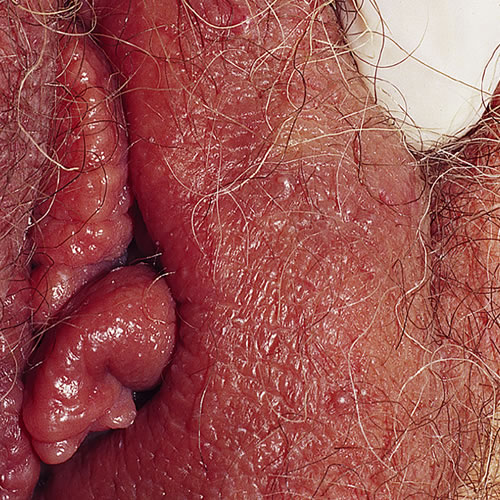
Erysipelas has an obvious margin that is raised and sharply demarcated from normal skin. It is painful. Fever and malaise may occur.
Diagnosis
The diagnosis is clinical. Culture helps in only 25% of the cases.
Pathology/Laboratory Findings
Biopsy of the leading edge of inflammation can identify the pathogen only 20% of the time, but may be useful to rule out dermatosis.
Differential diagnosis
Contact dermatitis, urticaria, fixed drug eruption, and herpes zoster.
Treatment/management
The following drugs are recommended:
- Cloxacillin 0.5 to 1 g orally every 6 hours x 7 to 10 days
- Erythromycin 500 g orally every 6 hours x 7 to 10 days
- For chronic recurrent disease, long-term penicillin (penicillin V potassium 300 to 500 mg orally four times a day for weeks, tapering to one dose daily over 3 to 6 months) is prescribed.
For associated lymphedema, see the section on vulvar lymphedema.
See Methicillin resistant Staph aureus document for information on this topic.