Introduction
Scabies1 is a highly contagious, itchy, skin infestation, caused by the mite, Sarcoptes scabiei which is an obligate human parasite.

Epidemiology
The incidence is estimated at 300 million cases per year worldwide.2 There used to be epidemics in cycles, but the latest epidemic is holding strong since the 1960’s.
The infestation occurs in children, young adults, and the institutionalized elderly most commonly. The mites spread by skin-to-skin contact but also by fomites such as clothing, toilet seats, etc. In some areas of Central and South America, prevalence is about 100%.3
A synonym for chronic, undiagnosed scabies is “seven-year itch.”
Etiology
Sensitization to S. scabiei (which will manifest, finally, in pruritus) takes several weeks to develop after the first infestation.4Subsequent infestations will result in pruritus within 24 hours. Immunocompromised patients, or those with neurologic disorders (Down syndrome, dementia, strokes, spinal cord injury, neuropathy, etc) may have the more extensive, crusted type of infestation, which results in a higher ratio of mites; this exacerbates symptoms and increases the risk of infecting others. Nodular scabies is seen more often in children.5
Symptoms and clinical features
Patients can report minor irritation and slightly itchy skin to very itchy skin and scratching. Nocturnal itching is typical. The head and neck are often spared in adults, but not in infants. Half of the people who have the crusting type of infestation do not have itching.6
An examination shows typical tiny erythematous papules, vesicles, and small jagged linear burrows in body creases, particularly finger webs, wrists, and axillary folds. In women, the breasts, buttocks, and inframammary folds are commonly involved, but the vulva often escapes. As the condition becomes more chronic, the lesions can become papular and then nodular. Some of these nodules may persist even after treatment. In infants, there may be involvement of the scalp and face. In the elderly, there may be more excoriations than true papules or nodules. Some people have itch alone, with no skin lesions.
The onset is insidious with minor irritation and slightly itchy skin that gradually worsens. Symptoms start within 21 days for initial infestation, within 1-3 days for re-infestations. Secondary eczematous dermatitis may occur, as may secondary infection.
Diagnosis
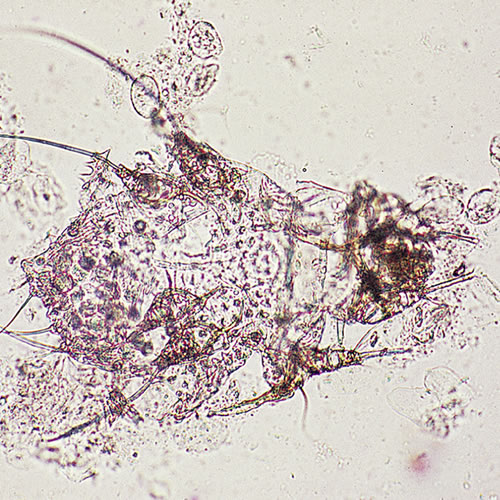
The diagnosis rests on the clinical pattern, isolation of a mite and/or a confirmatory skin scraping. There can be secondary infection, especially with MRSA. Biopsy, if done, will reveal the mites or the eggs.
Pathology/Laboratory Findings
To test skin scrapings, use 10% KOH dropped on the scrapings on a glass slide under a cover slip. Examine the slide under the microscope for the typical mite and eggs.
Differential diagnosis
Differential diagnosis includes folliculitis, neurodermatitis, atypical tinea, and contact dermatitis.
Treatment/management
All patient contacts need to be treated at the same time. All clothing, bedding, etc. is washed at 60° C and kept away from human skin for 72 hrs. Medication options include:
- Permethrin 5% (Nix or Elimite) cream is applied thinly to all areas of the body from the neck down and left on for 8 to 12 hours, then washed off. Retreatment after one month may occasionally be needed. Adverse events are rare. May be used in pregnant/lactating women and young children.
- Lindane 1% lotion is applied thinly to all areas of the body from the neck down and left on for 8 to 12 hours, then washed off. It may be reapplied in 24 hours or in 7 days to minimize recurrences or failures, although there is no study that proves that two applications are better than one.7 Resistance has been reported. Seizures and aplastic anemia after lindane use have also been reported.
Note: This is not to be used in pregnant or lactating women, in children under 2 years of age or in people with extensive dermatitis.
- Precipitated sulfur in petrolatum or a cold cream base (6% for children, 10% for adults) is applied from chin to toes twice a day for 2 days.
- Ivermectin is an oral antihelmintic used primarily to treat worm infections and river blindness. It has been used successfully, however, in the treatment of scabies that is not responsive to topical medications. One dose is effective.
Ivermectin is contraindicated in children under the age of five, or those that weigh less than 15 kg (33 lb) and those who are breastfeeding, and have a hepatic or renal disease8 - There are other possible treatments which should be handled by a dermatologist, particularly in the case of crusted scabies or extensive infestation.
For the rash of scabies after the treatment or for secondary dermatitis, a midpotency corticosteroid ointment can be used twice a day until the rash has subsided. It is important to note that prolonged use of a steroid ointment prior to proper diagnosis can lead to worsening of the condition due to suppression of the immune response.
An antihistamine such as hydroxyzine hydrochloride 10 to 25 mg at bedtime can be given for itching. Itching may be prolonged even after treatment.
Because of the risk of superinfection with scabies, methicillin resistant Staph aureus must always be considered. MRSA.
References
- Fisher BK, Margesson, LJ. Genital Skin Disorders: Diagnosis and Treatment. Mosby, Inc., 1998.150-151.
- Wolff K, Johnson RA. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology, sixth edition. McGraw Hill Medical 2009. 869.
- Wolff K, Johnson RA. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology, sixth edition. McGraw Hill Medical 2009. 869.
- Wolff K, Johnson RA. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology, sixth edition. McGraw Hill Medical 2009. 869.
- Wolff K, Johnson RA. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology, sixth edition. McGraw Hill Medical 2009. 869.
- Wolff K, Johnson RA. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology, sixth edition. McGraw Hill Medical 2009. 869.
- Wolff K, Johnson RA. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology, sixth edition. McGraw Hill Medical 2009. 874.
- Dourmishev AL, Dourmishev LA, Schwartz RA.Ivermectin: pharmacology and application in dermatology. International Journal of Dermatology. December 2005. 44 (12): 981–988.