Introduction
A melanocytic nevus1 is a small, circumscribed, variably pigmented macule or papule made up of nests of melanocytic cells derived from the embryological neural crest.
Synonyms include mole, nevocellular nevus, nevus pigmentosus, and acquired melanocytic nevocellular nevus.
Epidemiology
About 15% of women have pigmented lesions in the vulvar area,2 most developing in childhood or adolescence. Of these, 35-50% are melanocytic nevi, usually benign. Junctional and compound melanocytic nevi are usually found in childhood and teen years while dermal nevi manifest when patients are in their 30’s or 40’s.3
Etiology
Melanocytes normally occur in the basal layer of the epidermis in every fourth to tenth cell as well as in hair follicles.4 It is not known why the melanocytic nests develop to form these lesions. Genetic factors may play a role.
Melanocytic nevi can occur in the vulvar skin at the following levels:
Junctional nevi: cells at the dermal-epidermal junction above the basement membrane.
Compound nevi: combination of junctional and intradermal nevi.
Dermal nevi: cells in the dermis only.
Symptoms and clinical features
Nevi are often noted not by the patient but by the caregiver, and the patient is referred to rule out neoplasia. Sometimes, the patients may notice a lesion that is changing in color or size. Occasionally, the lesions may be traumatized and irritated by clothing or accidentally scratched and ulcerated.
Dermatological researchers believe that nevomelanocytic nevi are in a state of evolution in which they gradually transform over time from
junctional- cells at the dermoepidermal junction above the basement membrane
intradermal nevi- cells in the dermis only
compound nevi – combination of junctional and intradermal nevi
The different types of nevi have different morphological characteristics:
Flat nevi: usually junctional, usually uniform light brown to brown-black pigmentation
Slightly elevated nevi: compound or junctional, usually uniform light brown to brown-black pigmentation
Mucosal nevi: usually junctional
Papillomatous nevi: mostly intradermal, flesh colored to brown with a pebbly surface
Dome-shaped nevi: intradermal, flesh colored to brown with a smooth or pebble surface
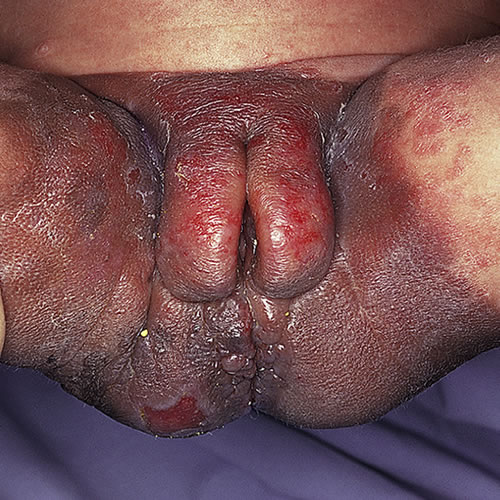
Pedunculated nevi: intradermal
Dysplastic nevi: flat or elevated, speckled pigmentation, irregular shape, reddish hues and indistinct margins

Giant congenital nevomelanocytic nevi: rare, usually presenting at birth as a sharply demarcated, hyperpigmented plaque studded with papules and nodules of varying sizes and degrees of pigmentation, usually over the lower back and hips, hence ‘bathing trunk’ nevus; melanoma risk is about 6.3%.
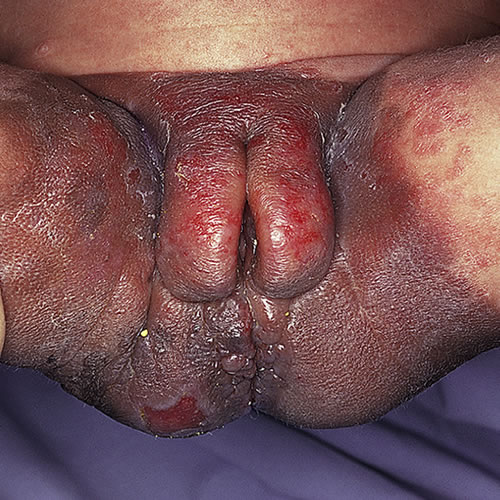
Common, benign nevi are regular in shape and consistent in coloration, with sharply demarcated borders. They are usually under 6-7 mm in diameter. Many melanocytic nevi have at least one atypical feature such as slight variation in pigmentation tone or a slightly irregular edge. More than one atypical feature may indicate an atypical or dysplastic lesion. That is why diagnosis must, in most cases, be made through biopsy or excision to be reliable.

Diagnosis
Diagnosis is made based on clinical appearance and histopathology.
Pathology/laboratory findings
Histological findings can distinguish between benign and malignant melanocytic lesions when the naked eye cannot.
Differential diagnosis
Differential diagnosis includes seborrheic keratosis, warts, VIN, melanoma, and basal cell carcinoma.
Treatment/management
No treatment is needed for obviously benign nevi unless there is repeated trauma resulting from their size and site. Then surgical removal is necessary. All suspicious lesions should be excised by either a shave excision or a simple excision with suture closure. Up to 20% of malignant melanomas arise in preexisting nevi, usually junctional or compound. If there is any question, always do an excisional removal for histopathology.
If no treatment is undertaken, patients need to be aware of their nevi and instructed to monitor them for changes.
References
- Fisher BK, Margesson, LJ. Genital Skin Disorders: Diagnosis and Treatment. Mosby, Inc., 1998. 188-189.
- Barnhill RL, Albert LS, Shama SK, et al. Genital lentiginosis: a clinical and histologic study. J Am Acad Dermatol. 1990;22:453-460.
- Wolff K, Johnson RA. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology, sixth edition. McGraw Hill Medical, 2009. 179.
- Heller DS, Wallach RC (ed.) Vulvar Disease: a Clinicopathological Approach. Informa Healthcare USA, Inc., 2007. 115