Introduction
Melanoma1 is a malignant neoplasm of melanocytes with generally poor prognosis. Melanomas of the vulva, vagina, and anorectal region are considered mucosal melanomas (MM) and are different from cutaneous melanomas (CM) in many ways. Mucosal melanomas comprise less than 2% of all melanomas. Anorectal melanomas occur in 1% of all melanomas, while vulvar and vaginal lesions occur in less than 1%. Of all MM, 25-30% are anorectal and 15-20% are vulvar or vaginal.2
Epidemiology
Vulvar melanomas (VuM), (more common (95% vs 3%) than vaginal melanomas (VaM), are the second most common vulvar malignancy after squamous cell carcinoma. They represent 5 to 10 percent of all malignant tumors involving the vulva, but less than 1 percent of all melanomas.3 The incidence of vulvar melanoma is 0.1 in 100 000.4 Anorectal melanoma has an incidence of approximately 0.4 per 1 000 000 in both men and women,5 usually occurring in the seventh decade. Anorectal melanoma has an increasing incidence, whereas the incidence of VuM is decreasing.6 Anorectal melanoma is found in 5% of all anal cancers, mainly located in the anal canal and presenting most frequently in Caucasian women in their 60’s and 70’s.7
Vulvar melanomas occur more commonly in postmenopausal white women and are thicker and larger at the time of diagnosis than melanomas diagnosed elsewhere. A patient with a vulvar melanoma is usually 45 to 65 years of age, but may present with lesions into her 80’s.8 Primary melanoma of the vagina is 5-9 times less common than primary melanoma of the vulva and is, like anorectal melanoma, more difficult to see and diagnose.
Etiology
CM and MM are different in many ways9 and more than one report indicates that VuM may be unique in its molecular profile.10 Whereas cutaneous melanomas are strongly related to sun exposure, no clear environmental or other risk factors have been identified in the vulvovaginal form of the disease. However, it has been suggested that ultraviolet radiation may be involved in modifying immunity and that may affect development of tumors.11
Genetic predisposition may play a role in acquisition of MM, but there are no studies that prove this, just as there is no proof of other particular risk factors.
Symptoms and clinical features
It is incumbent upon clinicians to check for these mostly pigmented lesions because patients often do not notice them until the condition reaches an advanced stage, presenting as a lump or mass, with bleeding or itching. (Less frequently, patients present with a “changing mole.”)
Primary melanoma of the vagina is usually found in the lower third of the vaginal canal on the anterior wall and may present as a single or as multiple pigmented or non-pigmented lesion(s).12 Primary melanoma of the vulva usually presents on the labia majora (50%), the labia minora (<20%), the clitoris (10-15%), and the Bartholin glands (<5%).13
| Clinico/histological types of melanoma |
|---|
| Superficial Spreading Melanoma—a flat, pigmented, irregularly bordered macule or elevated, variegated brown, red, blue-gray to black plaque with a very irregular border that typically has a slow horizontal growth phase then a vertical growth phase with development of a nodule. It represents 50% of vulvar melanomas. |
| Nodular Melanoma—a rapidly growing melanocytic tumor with no horizontal growth phase, an aggressive vertical growth phase, and a poor prognosis. The color may be variegated, blue-black, reddish, or ulcerated. The two variants (nodular and nodular polypoid) of nodular melanoma together make up 35% of vulvar melanomas. |
| Acral Lentiginous Melanoma—a melanoma that occurs mostly on palms, soles, and nail beds, but may occur on the mucocutaneous skin of the mouth, genitalia, and anus. Sometimes, it has a discontinuous horizontal growth phase and is aggressive. Lesions may be black, brown, blue, with irregular or poorly defined margins. It is relatively rare in whites, occurring more commonly in Asians and in patients with brown or black skin. It accounts for 15% of melanomas of the vulva. |




Diagnosis
Clinical and histopathologic impressions determine the diagnosis. The ABCDE approach is useful for diagnosis, assessing asymmetry, border irregularity, color, diameter, and evolution (of size, shape, or color) of the lesion(s).14 15
VuM can resemble both benign lentiginosis (melanosis) and benign pigmented nevi (moles). (Well known vulvar dermatologist Libby Edwards says, “If it’s regular, it’s regular” in explaining her primary approach). Raising the suspicion of melanoma are larger lesions, asymmentrical lesions, those with border irregularity, speckling, or irregular coloration. They may be flat, raised, or nodular. There may be shades of red, black, gray, dark brown, blue and white. Amelanotic melanoma occurs in shades of pink or red. There may be ulceration.
Excisional biopsy of smaller and incisional or punch biopsy of larger suspicious lesions is of great importance for diagnosis. Recommendations for excisional margins range from 0.5 cm for localized, well-demarcated lesions to 1 cm for lesions up to 2 mm thick, and 2 cm for lesions thicker than 2 mm have been suggested, without survival benefit shown for margins greater than 2 cm.16 Each clinician should decide on a diagnostic action appropriate to his/her/their education, practice, and comfort level.
Prognosis is based on Clark’s levels of invasion, Breslow’s direct thickness measurement, and completeness of excision17 and on staging based on the American Joint Committee on Cancer (AJCC) melanoma staging system. This system takes into account multiple factors to predict treatment and survival outcomes.18
Pathology/Laboratory Findings
Excisional biopsy is done if adequate margins and appropriate depth can be guaranteed. If the lesion is too big, an incisional biopsy can be done without risk of seeding the tumor.
Differential diagnosis
Differential diagnosis includes benign nevus, VIN, and mucosal melanotic macule.
Treatment/management
Management and outcome depend on the histologic depth of the lesion, the completeness of removal, histopathological diagnosis, presence of involved groin lymph nodes, and staging. One study proposed that “vulval, vaginal, and cervical melanomas may differ in terms of their clinico-pathological features and associations with” both survival rates and risk of recurrence.19 Palpable lymph nodes can be needle-biopsied. Presence of disseminated disease may need to be assessed via MRI and/or CT or CT-PET.
Prognosis of vulvovaginal mucosal melanoma is poor (approximately 15% 5 year survival) because of the high metastatic potential of these lesions.20 21
Treatment is surgical, requiring the expertise of the gynecologic oncologist and often a multidisciplinary team to support the patient. Radical vulvectomy has fallen out of favor as the procedure of choice because it has not shown any benefit for long term survival. Rather, radical wide local excision with margins of at least 1 cm is preferred.22 Frozen sections can be used to ascertain ulcer margins in recurrent acral lentiginous lesions.
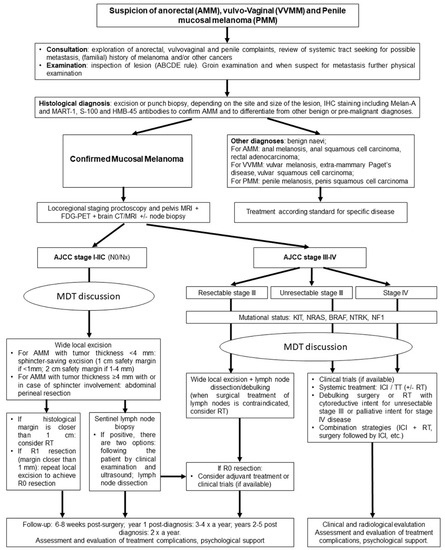
The following algorithm23 is a summary of an excellent article on the topic of mucosal melanomas.
Early superficial spreading melanomas less than 1.5 mm in depth of invasion have a relatively good outcome with radical wide local resection. These patients have the best chance for “cure.” Beyond that, surgery is combined with a variety of chemotherapeutic or radiotherapeutic modalities. The best treatment is an early diagnosis and local removal. Surgery, radiation, and chemotherapy may provide some helpful palliative treatment for larger lesions. Palpably positive groin lymph nodes should be removed to prevent groin skin ulceration in the palliative phase of care of advanced disease.
References
- Fisher BK, Margesson, LJ. Genital Skin Disorders: Diagnosis and Treatment. Mosby, Inc., 1998. 214.
- Ottaviano M, Giunta EF, Marandino L, Tortora M, Attademo L, Bosso D, Cardalesi C, Fabbrocini A, Rosanova M, Silvestri A, et al. Anorectal and Genital Mucosal Melanoma: Diagnostic Challenges, Current Knowledge and Therapeutic Opportunities of Rare Melanomas. Biomedicines. 2022; 10(1):150. https://doi.org/10.3390/biomedicines10010150
- Stang A, Streller B, Eisinger B, Jöckel KH. Population-based incidence rates of malignant melanoma of the vulva in Germany. Gynecol Oncol 2005; 96:216
- , , . Cancer of the vulva: 2021 update. Int J Gynecol Obstet. 2021; 155(Suppl. 1): 7-18. https://doi.org/10.1002/ijgo.13881
- Edwards L. and Lynch P. Genital Dermatology Atlas and Manual, 3rd edition. Wolters Kluwer, 2018. p 159.
- Edwards L and Lynch P. Genital Dermatology Atlas and Manual, 3rd edition. Wolters Kluwer, 2018. p 159.
- , , . Cancer of the vulva: 2021 update. Int J Gynecol Obstet. 2021; 155(Suppl. 1): 7–18. https://doi.org/10.1002/ijgo.13881
- , , . Cancer of the vulva: 2021 update. Int J Gynecol Obstet. 2021; 155(Suppl. 1): 7–18. https://doi.org/10.1002/ijgo.13881
- Coit D.G., Thompson J.A., Algazi A., Andtbacka R., Bichakjian C.K., Carson W.E., 3rd, Daniels G.A., DiMaio D., Ernstoff M., Fields R.C., et al. Melanoma, Version 2. 2016, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2016;14:450–473. doi: 10.6004/jnccn.2016.0051
- Wohlmuth C., Wohlmuth-Wieser I., May T., Vicus D., Gien L.T., Laframboise S. Malignant Melanoma of the Vulva and Vagina: A US Population-Based Study of 1863 Patients. Am. J. Clin. Dermatol. 2020;21:285–295. doi: 10.1007/s40257-019-00487-x.
- Mundra, P.A., Dhomen, N., Rodrigues, M. et al. Ultraviolet radiation drives mutations in a subset of mucosal melanomas. Nat Commun 12, 259 (2021). https://doi.org/10.1038/s41467-020-20432-5
- Ottaviano M, Giunta EF, Marandino L, Tortora M, Attademo L, Bosso D, Cardalesi C, Fabbrocini A, Rosanova M, Silvestri A, et al. Anorectal and Genital Mucosal Melanoma: Diagnostic Challenges, Current Knowledge and Therapeutic Opportunities of Rare Melanomas. Biomedicines. 2022; 10(1):150. https://doi.org/10.3390/biomedicines10010150
- Ottaviano M, Giunta EF, Marandino L, Tortora M, Attademo L, Bosso D, Cardalesi C, Fabbrocini A, Rosanova M, Silvestri A, et al. Anorectal and Genital Mucosal Melanoma: Diagnostic Challenges, Current Knowledge and Therapeutic Opportunities of Rare Melanomas. Biomedicines. 2022; 10(1):150. https://doi.org/10.3390/biomedicines10010150
- Abbasi N.R., Shaw H.M., Rigel D.S., Friedman R.J., McCarthy W.H., Osman I., Kopf A.W., Polsky D. Early diagnosis of cutaneous melanoma: Revisiting the ABCD criteria. Jama. 2004;292:2771–2776. doi: 10.1001/jama.292.22.2771.
- Wohlmuth C., Wohlmuth-Wieser I. Vulvar Melanoma: Molecular Characteristics, Diagnosis, Surgical Management, and Medical Treatment. Am. J. Clin. Dermatol. 2021;22:639–651. doi: 10.1007/s40257-021-00614-7.
- Mert, I.; Semaan, A.; Winer, I.; Morris, R.T.; Ali-Fehmi, R. Vulvar/Vaginal Melanoma. Int. J. Gynecol. Cancer 2013, 23, 1118–1126.
- Heller DS, Wallach RC (ed.) Vulvar Disease: a Clinicopathological Approach. Informa Healthcare USA, Inc., 2007.123-124.
- Gershenwald, J.E.; Scolyer, R.A.; Hess, K.R.; Thompson, J.F.; Long, G.V.; Ross, M.I.; Lazar, A.J.; Atkins, M.B.; Balch, C.M.; Barnhill,R.L.; et al. Melanoma of the Skin. AJCC Cancer Staging Man. 2016, 2017, 563–586.
- Wu Y, Li H, Tan L, Lai Y, Li Z. Different clinico-pathological and prognostic features of vulvar, vaginal, and cervical melanomas. Hum Pathol. 2023 Jan;131:87-97. doi: 10.1016/j.humpath.2022.11.002. Epub 2022 Nov 10. PMID: 36370822.
- Ottaviano M, Giunta EF, Marandino L, Tortora M, Attademo L, Bosso D, Cardalesi C, Fabbrocini A, Rosanova M, Silvestri A, et al. Anorectal and Genital Mucosal Melanoma: Diagnostic Challenges, Current Knowledge and Therapeutic Opportunities of Rare Melanomas. Biomedicines. 2022; 10(1):150. https://doi.org/10.3390/biomedicines10010150
- Olawaiye AB, Cuello MA, Rogers LJ. Cancer of the vulva: 2021 update. Int J Gynaecol Obstet. 2021 Oct;155 Suppl 1(Suppl 1):7-18. doi: 10.1002/ijgo.13881. PMID: 34669204; PMCID: PMC9298362.
- Nobbenhuis MA, Lalondrelle S, Larkin J, Banerjee S. Management of melanomas of the gynaecological tract. Curr Opin Oncol. 2014;26:508‐513. [PubMed] [Google Scholar]
- Ottaviano M, Giunta EF, Marandino L, Tortora M, Attademo L, Bosso D, Cardalesi C, Fabbrocini A, Rosanova M, Silvestri A, et al. Anorectal and Genital Mucosal Melanoma: Diagnostic Challenges, Current Knowledge and Therapeutic Opportunities of Rare Melanomas. Biomedicines. 2022; 10(1):150. https://doi.org/10.3390/biomedicines10010150