Introduction
Behçet disease1 is a rare, multi-system disorder that classically consists of the triad of oral ulcers, genital ulcers, and uveitis but is known to involve almost any organ system.
Epidemiology
Prevalence is high in the Middle East, the Mediterranean countries (especially Turkey), and Japan, but low in Western countries. It is difficult to distinguish this disease from complex aphthosis. It usually presents before the age of 40.2
Etiology
Unknown.
Symptoms and clinical features
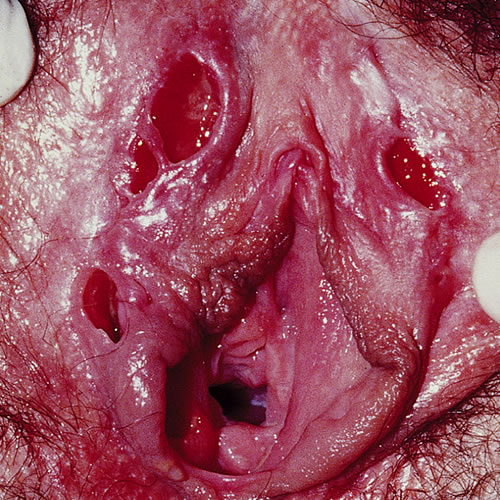
The most common presentation is multiple, recurrent, painful, oral aphthous ulcers (100% of cases). In the vulva, the presenting complaint may be dyspareunia with recurrent crops of multiple, very tender, genital ulcers that take 2 to 4 weeks to heal. The onset of the oral and genital ulcers can be associated with fever, malaise, and arthritis. Elsewhere on the skin, folliculitis, furuncles, and a pustular dermatitis occur wherever there is skin trauma. Erythema nodosum and erythema multiforme have also been associated with this condition. Associations that are more serious are thrombophlebitis and central nervous system changes such as stroke, aneurysm, paralysis, nerve palsies, and psychosis.
Aphthous ulcers in the mouth present typically as small punched-out canker sores on the buccal mucosa and tongue and can be extensive (even on the pharynx) with a pseudo-membranous coating. In the vulvar area, the 2 mm to 30 mm lesions can be individual and punched-out, but often form multiple, contiguous, sharply demarcated ulcers with fibrinous bases and considerable undermining that can eventually lead to sinus formation, fenestration, and partial or complete destruction of the labia.
Pathology/Laboratory Findings
Biopsy may yield leukocytoclastic vasculitis with fibrinoid necrosis of blood vessel walls in acute early lesions and lymphocytic vasculitis in late lesions.Wolff K and Johson, RA. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology, sixth edition. McGraw Hill Medical. 2009. 366.
Diagnosis
Diagnosis is made on the fulfillment of clinical criteria — recurrent oral ulceration plus two of the following:
- Recurrent genital ulceration
- Eye lesions (uveitis or retinovasculitis)
- Skin lesions (erythema nodosum, folliculitis, acneiform nodules)
- Positive pathergy tests (intradermal injection of sterile water that results in the formation of a papule or pustule in 48 hours).
Differential diagnosis
Crohn disease, herpes simplex in the immunosuppressed, chancroid, granuloma inguinal, tuberculosis, syphilis, celiac disease, and lymphogranuloma venereum.
Because the ulcers may resemble other ulcers and to help in the diagnosis of generalized disease, the following tests should also be done:
- Herpes I & II titers; herpes culture; testing for other ulcers that may be prevalent in your area.
- Zinc serum, Vit B 12, iron serum, hemogram, folate RBC, Transglutaminase AB IGA
- Yeast culture
- Biopsy edge of ulcer
Treatment/management
Management depends on the extent of involvement. Treatment should be guided by an experienced dermatologist or gynecologist.
Provide local care: warm soaks, patting dry, no tight clothing, etc.
For mild vulvar ulceration, recommend gentle cleansing with Cetaphil cleanser or Basis soap to be followed by a superpotent steroid (Halobetasol or Clobetasol 0.05% ointment applied in a thin film bid for 1 to 2 weeks or more, while lesions are present). For local discomfort, the patient can use a topical EMLA cream applied for 15 to 20 minutes under plastic wrap occlusion
Specific Treatment. The following treatments have been used separately and in combination.
- For localized involvement, use intralesional cortisone, triamcinolone acetonide (Kenalog-10) mixed 1:2 with saline and injected after applying EMLA topical anesthesia.
- Prednisone 20 to 60 mg/day orally. One specialist uses Prednisone 40-60 mg orally every morning for 7-10 days. 3
- Colchicine 0.6 mg orally three times a day or less is good for limited disease and as a steroid sparer.
- Dapsone 100 mg/day orally. It can be used along with colchicine or by itself as a steroid sparer. Before use, check the patient’s glucose-6- phosphate dehydrogenase (G-6-PD) level to rule out G-6-PD deficiency. 4
- Azathioprine 1 to 2 mg/kg/day orally for patients unresponsive to prednisone.
- Thalidomide (available on a restricted basis) 50 to 200 mg/day orally. 5
- Methotrexate 7.5 to 20 mg/week orally for resistant disease.
- Cyclosporine 3 to 5 mg/kg/day orally.
Note: All cytotoxic drugs require careful adherence to monitoring guidelines
References
- Fisher BK and Margesson LJ. Genital Skin Disorders: diagnosis and treatment. Mosby, 1998. 159-160.
- Wolff K and Johson, RA. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology, sixth edition. McGraw Hill Medical. 2009. 366.
- Edwards L, Lynch P. Genital Dermatology Atlas, second edition. Wolters Kluwer/Lippincott Williams & Wilkins. 168.
- Letsinger JA, McCarty MA, Jorizzo JL. Complex aphthosis: a large case series with evaluation algorithm and therapeutic ladder from topical to thalidomide. J Am Acad Dermatol. 2005; 52:500-508.
- Mimura MAM, Hirota SK, Sugaya NN, et al. Systemic treatment in severe cases of recurrent aphthous stomatitis: an open trial. Clinics (Sao Paulo). 2009; 64(3): 193-198.