Introduction
A Bartholin gland cyst1 is a common vulvar cyst that develops from blockage of one of the two major vulvar vestibular glands. Infection of the cyst leads to an abscess.
Epidemiology
One to two percent of women get these cysts, mostly during their 30’s.
Etiology
This cyst forms when the Bartholin gland duct becomes obstructed secondary to nonspecific inflammation or trauma. These ducts are easily obstructed, usually near the distal orifice.2 Following blockage, there is continued secretion of glandular fluid leading to cystic dilation. These common cysts, when small, may be asymptomatic.
Symptoms and clinical features
Symptoms develop as the cysts enlarge or become infected. Sitting or walking may then be difficult because they are extremely painful. There may be pain with intercourse. Signs of systemic infection may develop.
These round or ovoid cysts, usually unilateral, in the lower lateral labium minor at the 5 or 7 o’clock positions just anterior to the hymenal ring, are usually 1 to 4 cm but may become as large as 8 cm in diameter.
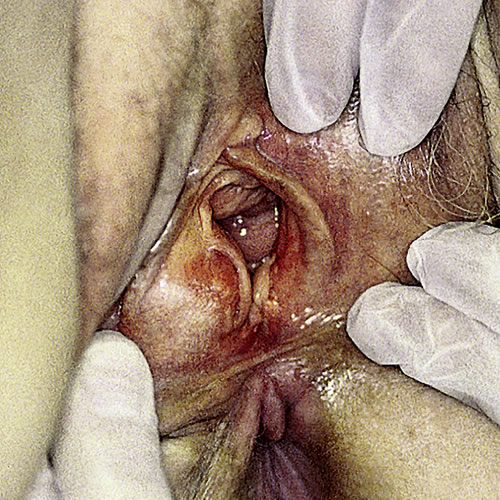
Infection with the usual skin organisms (and in some cases Neisseria gonorrhoeae) results in marked erythema and exquisite tenderness. The whole introital area can be blocked with the edematous and erythematous swelling. Often, the bulging tissue occurs directly under the labium minus on one side.


Diagnosis
Diagnosis is clinical. The cysts cause a soft, painless mass unless they are inflamed. They are usually filled with clear, sterile fluid. Abscesses may be warm to the touch, tender, and fluctuant, surrounded by edema and cellulitis, and may drain pus spontaneously to some extent.
Pathology/Laboratory Findings
Biopsy is not necessary unless there is a question of malignancy represented by a solid mass or skin lesion. Women over 40 may need pathological evaluation because there is a small risk of cancer of the Bartholin gland in older women. The organisms that may cause infection are Staphylococcus species, Streptococcus species, Bacteroides species, Escherichia coli, Chlamydia trachomatis, and Neisseria gonorrhoeae. Culture should be done if pus is present in the cyst.3 Methicillin-resistent Staph aureus (MRSA) needs to be considered for any skin abscess. (MRSA).
Differential diagnosis
Epidermal cyst, lipoma, and fibroma.
Treatment/management
Asymptomatic, small cysts require no treatment. Abscesses that drain spontaneously may only need pain medication and warm soaks. Infected abscesses need treatment with antibiotics. Abscesses should be drained under local anesthesia, usually in the office setting. Incision and drainage has a risk of recurrence. Placement of a Word catheter has less likelihood of recurrence but includes the risk of being dislodged during the month it must stay in place to allow healing.
“Marsupialization” (actually unroofing) of the cyst or abscess cavity, with surgical eversion of tissue to keep a new channel for drainage open, can be done; it has a recurrence rate of 5-20%.4 Complete removal of the cyst or abscess by surgical excision in an operating room may be necessary. Complications include bleeding, hematoma, scarring, and pain. Laser treatment can be done if available.
References
- Fisher BK and Margesson MJ. Genital Skin Disorders; diagnosis and treatment. Mosby, 1998. 196-197.
- Eckert LO, Lentz GM. Infections of the lower genital tract. In: Katz VL, Lentz GM, Lobo RL, Gershenson DM, eds. Comprehensive Gynecology, 5th ed. Philadelphia, Mosby Elsevier, 2007, 572.
- Edwards L and Lynch P. Genital Dermatology Atlas, second edition. Wolters Kluwer Health/Lippincott Williams and Wilkins, 2011. 208.
- Wechter NE, Wu JM, Marzano D, et al. Management of Bartholin duct cysts and abscesses: a systematic review. Obstet Gynecol Surv. 2009; 64:395-404.